-
PDF
- Split View
-
Views
-
Cite
Cite
Rolando Herrero, Xavier Castellsagué, Michael Pawlita, Jolanta Lissowska, Frank Kee, Prabda Balaram, Thangarajan Rajkumar, Hema Sridhar, Barbara Rose, Javier Pintos, Leticia Fernández, Ali Idris, María José Sánchez, Adoración Nieto, Renato Talamini, Alessandra Tavani, F. Xavier Bosch, Ulrich Reidel, Peter J. F. Snijders, Chris J. L. M. Meijer, Raphael Viscidi, Nubia Muñoz, Silvia Franceschi, For the IARC Multicenter Oral Cancer Study Group, Human Papillomavirus and Oral Cancer: The International Agency for Research on Cancer Multicenter Study, JNCI: Journal of the National Cancer Institute, Volume 95, Issue 23, 3 December 2003, Pages 1772–1783, https://doi.org/10.1093/jnci/djg107
Close - Share Icon Share
Abstract
Background: Human papillomavirus (HPV), the causal agent of cervical cancer, appears to be involved in the etiology of cancer of the oral cavity and oropharynx. To investigate these associations, we conducted a multicenter case-control study of cancer of the oral cavity and oropharynx in nine countries. Methods: We recruited 1670 case patients (1415 with cancer of the oral cavity and 255 with cancer of the oropharynx) and 1732 control subjects and obtained an interview, oral exfoliated cells, and blood from all participants and fresh biopsy specimens from case patients. HPV DNA was detected by polymerase chain reaction (PCR). Antibodies against HPV16 L1, E6, and E7 proteins in plasma were detected with enzyme-linked immunosorbent assays. Multivariable models were used for case-control and case-case comparisons. Results: HPV DNA was detected in biopsy specimens of 3.9% (95% confidence interval [CI] = 2.5% to 5.3%) of 766 cancers of the oral cavity with valid PCR results and 18.3% (95% CI = 12.0% to 24.7%) of 142 cancers of the oropharynx (oropharynx and tonsil combined) with valid PCR results. HPV DNA in cancer biopsy specimens was detected less frequently among tobacco smokers and paan chewers and more frequently among subjects who reported more than one sexual partner or who practiced oral sex. HPV16 DNA was found in 94.7% of HPV DNA-positive case patients. HPV DNA in exfoliated cells was not associated with cancer risk or with HPV DNA detection in biopsy specimens. Antibodies against HPV16 L1 were associated with risk for cancers of the oral cavity (odds ratio [OR] = 1.5, 95% CI = 1.1 to 2.1) and the oropharynx (OR = 3.5, 95% CI = 2.1 to 5.9). Antibodies against HPV16 E6 or E7 were also associated with risk for cancers of the oral cavity (OR = 2.9, 95% CI = 1.7 to 4.8) and the oropharynx (OR = 9.2, 95% CI = 4.8 to 17.7). Conclusions: HPV appears to play an etiologic role in many cancers of the oropharynx and possibly a small subgroup of cancers of the oral cavity. The most common HPV type in genital cancers (HPV16) was also the most common in these tumors. The mechanism of transmission of HPV to the oral cavity warrants further investigation.
Cancers of the oral cavity and oropharynx constitute major worldwide public health problems, with more than 400 000 new cases expected for 2005, if current incidence rates remain unchanged (1,2). Tobacco and alcohol are established etiologic agents of these cancers (3), with attributable fractions of approximately 90%. Micronutrient deficiencies (4,5) and poor oral hygiene (6) have also been associated with increased risk.
Human papillomavirus (HPV) is etiologically involved in virtually all cervical cancers [for review, see(7)], and the early HPV oncoproteins E6 and E7 are responsible for the malignant phenotype, mainly through inactivation of tumor suppressor proteins such as p53 and pRB. Previous work evaluating different markers of exposure and viral activity in tumors indicates that HPV may also play a role in some cancers of the oral cavity and oropharynx (8). Several studies [(9–11); for review, see (12)] have investigated prevalence of HPV in these cancers, but the prevalence of HPV detection varies broadly, depending on the population, combination of subsites, type of specimen, and detection method. HPV is consistently and more frequently detected in cancers of the oropharynx and tonsil than at other head and neck sites, and HPV16 tends to be the predominant type detected (9–11). Results of a few case-control studies (10,11) and a cohort study (13) point to a likely role of HPV in some cancers at certain anatomical sites. However, many aspects of the association remain to be investigated to better define the precise contribution of HPV to the etiology of these tumors and the potential preventive interventions (14).
We report an International Agency for Research on Cancer (IARC) multicenter case-control study of cancer of the oral cavity and oropharynx carried out in nine countries that used a common protocol for data and specimen collection and included several markers of HPV infection that were assayed in central laboratories.
Materials, Patients, and Methods
The study was conducted in Italy, Spain, Northern Ireland, Poland, India, Cuba, Canada, Australia, and Sudan from April 1996 through December 1999. Case patients were recruited as follows: in Italy, from three cancer referral hospitals in the Friuli-Venezia-Giulia and Lombardia regions (6); in Spain, from two hospitals in Barcelona, one in Granada, and one in Seville (3,5); in Northern Ireland, from the School of Dentistry and several general and cancer hospitals in Belfast; in Poland, from one maxillofacial surgery clinic in Warsaw (15); in India, from one cancer referral center each in Madras, Bangalore, and Trivandrum (16); in Cuba, from the main cancer referral center in Havana (4); in Canada, from three hospitals in Montreal; in Australia, from one cancer referral center in Sydney; and in Sudan, from a dental hospital in Khartoum. Control subjects were recruited in most centers from the same hospitals or neighboring general hospitals serving the same populations to which the case patients belonged. In Northern Ireland and India, selection of control subjects was modified so that they were recruited only if, in the event of a cancer diagnosis, they would have been admitted to the same hospitals in which the case patients were recruited (see below).
Case patients with incident cancer of the oral cavity or oropharynx were contacted at participating centers before any cancer treatment. Topographic locations included the lip (excluding the external lip), base of the tongue, other parts of the tongue, gum, floor of the mouth, palate, other parts of the mouth, tonsil, and oropharynx. Cancers of the oropharynx and tonsil were combined as oropharynx, and cancers at other sites were grouped as oral cavity (see below). Patients with second primary cancers were not eligible, and only carcinomas (including six adenocarcinomas) were included according to the local pathologist’s diagnosis. All cancers of the salivary gland and five lymphomas and one sarcoma of the other oral sites were excluded.
In most centers, one hospital control subject per case patient was selected and frequency-matched on center, sex, and 5-year age group. Control subjects were ineligible if they were mentally or physically unable to give consent, had a history of cancer of the oral cavity or oropharynx, or had a diagnosis associated with the exposures of interest. For example, potential control subjects with tobacco- and/or alcohol-related diseases (such as cancers of the lung, larynx, esophagus, bladder, kidney, liver, or pancreas; chronic lung diseases; coronary heart diseases; venous thrombosis; hepatitis; or cirrhosis) were not eligible. Patients with cancers of the anogenital tract, skin, or unknown primary site were also excluded. When patients with cancers with topographies not in the exclusion criteria were recruited as control subjects, they were recruited before any primary treatment and should not account for more than 20% of the overall comparison group. In India, control subjects were selected among patients without cancer presenting for voluntary cancer checkup or among visitors of patients with diseases other than cancer of the oral cavity or oropharynx (16). In Northern Ireland, community control subjects were selected from county listings, geographically matched to the case patients, and invited by personal letter.
We recruited 1670 case patients (1415 with cancer of the oral cavity and 255 with cancer of the oropharynx) and 1732 control subjects in nine countries. The study was approved by the IARC and local ethical review committees, and participants gave written informed consent according to local regulations.
Data and Specimen Collection
Specially trained interviewers administered a standardized questionnaire that included demographic characteristics (age, sex, ethnic group, area of birth and residence, religion, and language spoken), education (ever attendance at school, number of years of school attendance, and age when stopped going to school), longest occupation, use of tobacco in its different forms, alcohol drinking habits, dietary habits, marital status, sexual history (number of lifetime sexual partners, visits to prostitutes, and frequency of oral sex), histories of various diseases, family history of cancer, and oral cavity health. A smoker was defined as a subject who reported having smoked tobacco daily for at least 1 year, and smokers were asked about duration of smoking and amount and type of tobacco smoked (cigarettes, cigars, or pipes). In India, specific questions were asked about paan chewing (usually including tobacco, betel leaf, areca nut, and calcium hydroxide). Additional questions were asked about consumption of snuffed tobacco in some areas (e.g., toombak dipping in Sudan). A drinker was defined as a subject who reported drinking alcoholic beverages at least once a month, and details were obtained on type of beverage, amount, and duration.
Interviewers also briefly examined the oral cavity to determine the number of missing teeth and the presence of visible lesions. The association of oral cancer with some of the risk factors has been previously reported for some centers (3–6,15,16).
Before initiating the study in each center, extensive discussions with the local investigators were conducted, and questionnaires were modified to adapt them to the local culture or habits (e.g., so that they asked about toombak dipping in Sudan, betel quid chewing in India, and cigar smoking in Cuba). However, the core questionnaire was maintained to allow pooling of the main data. During the course of the study, the local investigators closely supervised the interview and specimen collection processes. In addition, the IARC investigators visited study sites before initiation of the study and periodically visited the main centers to ensure adherence to the common international protocol.
After administering the interview, information on tumor-node-metastasis classification and histology was obtained from case patients. This classification was converted into stage according to the American Joint Committee on Cancer (AJCC) Cancer Staging Manual (17). Superficial scrapes of the mucosa were carried out with soft toothbrushes, by performing 5–10 gentle strokes in predefined areas as follows: right buccal mucosa (from high to low position), left buccal mucosa (from high to low position), right side of the tongue, dorsal side of the tongue, left side of the tongue, and inside of the upper and lower lip, in addition to the gentle brushing of the tumor in case patients. Cells from brushes were suspended in tubes containing phosphate-buffered saline (PBS). Participants subsequently gargled with saline, and the resulting suspension was added to the same tube. Cells were centrifuged twice and frozen at −70 °C until shipment to Lyon (France) and then to Amsterdam (The Netherlands) for HPV testing.
Attempts were made to obtain a biopsy specimen from each case patient from a non-necrotic area of the tumor before any cancer treatment, although priority was given to biopsy examination required for diagnostic purposes. Biopsy specimens were placed in liquid nitrogen or in freezers at −70 °C or, in some areas, kept on ice or at 4 °C until later, always within 8 hours of collection. Specimens were shipped on dry ice to Lyon, where they were stored at −70 °C until shipment to Amsterdam for HPV testing.
A 10-mL heparinized blood sample was obtained, and aliquots of plasma were prepared and frozen until shipment on dry ice to Lyon. In Lyon, they were stored at −20 °C until transfer to collaborating laboratories in Heidelberg, Germany, and Baltimore, MD.
DNA Analysis
For polymerase chain reaction (PCR), suspensions of exfoliated cells and biopsy specimens were subjected to freezing-thawing and to boiling, as described (18). Snap-frozen biopsy specimens were serially sectioned (10–15 sections) on a cryostat. The first and last sections were stained with hematoxylin-eosin for histologic assessment of the presence of carcinoma. Intermediate sections were used for crude DNA extraction, as described (19). β-Globin PCR analysis was performed (20) to confirm the presence of human DNA in specimens; specimens with negative results were considered to not have valid PCR results and were excluded from subsequent analyses. Histologic assessment was possible in 89.3% (811) of the 908 biopsy specimens with valid PCR results. Of those 811 specimens, a total of 22.6% (183 specimens) were not adequate for histologic assessment (83 specimens) or apparently had no neoplastic cells (100 specimens). However, our estimates of detection of HPV DNA in biopsy specimens did not vary according to the apparent presence or absence of cancer in the specimen. Because all subjects had histologically confirmed cancers, we decided to include them all in the analyses.
For HPV DNA detection, the general primer (GP)-mediated PCR enzyme immunoassay (GP5+/biotinylated GP6+ PCR—EIA) was performed (19). PCR products were subsequently characterized in the following two ways: 1) EIA with two mixtures of oligonucleotide probes specific for 14 high-risk HPV types (HPV16, 18, 31, 33, 35, 39, 45, 51, 52, 56, 58, 59, 66, and 68) and six low-risk HPV types (HPV6, 11, 40, 42, 43, and 44) and 2) agarose gel electrophoresis followed by low-stringency Southern blot hybridization with a probe mixture containing general primer PCR products specific for HPV6, 11, 16, 18, 31, and 33 (21). Southern blot analysis was performed under low-stringency conditions to allow the detection of HPV types not included in the EIA probe mixtures. When the EIA was positive, subsequent typing was performed with EIA oligonucleotide probes individually. In this study, no sample with a negative EIA result had a positive hybridization result.
HPV testing of exfoliated cells was performed in 45.2% of case patients and 40.0% of control subjects from some of the centers (Table 1). The coordinating group decided not to continue testing exfoliated cell specimens and to focus on biopsy material when we observed the lack of association between HPV DNA detected in cells and HPV DNA in biopsy specimens (see below).
Detection of Antibodies Against HPV16 L1
Preparative purification of HPV16 virus-like particles.
For production of virus-like particles (VLPs), Trichoplusia ni (High Five) cells (Invitrogen, Carlsbad, CA) were infected with HPV16 L1/L2 recombinant baculovirus, clone 114/K (a gift from John T. Schiller, National Cancer Institute, Bethesda, MD) and grown as adherent cultures in tissue culture plates. VLPs were purified from cell lysates by density gradient ultracentrifugation, POROS 50 HS cation-exchange chromatography (PerSeptive Biosystems, Framingham, MA), and heparin-Sepharose chromatography (Amersham Pharmacia Biotech, Piscataway, NJ), as described previously (22).
HPV 16 VLP-based enzyme-linked immunosorbent assay.
Plasma was tested for antibodies to HPV16 VLP in an enzyme-linked immunosorbent assay (ELISA), as described previously (22). Briefly, 50 ng of VLP protein in PBS (pH 7.2) was incubated in wells of PolySorp microtiter plates (Nunc, Naperville, IL) overnight at 4 °C and then blocked for 3 hours at room temperature with 10% Superblock (Pierce, Rockford, IL) in PBS containing 0.05% Tween 20 (blocking buffer). Blocking buffer was replaced with PBS, and plates were stored at −20 °C until use. Before use and following each incubation step, the plates were washed four times with PBS containing 0.05% Tween 20 (Sigma-Aldrich, St. Louis, MO) in an automatic plate washer (Skanwasher 300; Skatron, Lier, Norway). Plasma samples were diluted 1 : 100 in blocking buffer, 100 μL of this diluent was added to duplicate wells, and the microtiter plates were incubated for 1 hour at 37 °C. Antigen-bound immunoglobulin was detected with peroxidase-conjugated goat antibodies against human immunoglobulin G (IgG; Zymed, San Francisco, CA) and diluted 1 : 4000 in a solution of 10% Superblock, 2.5% polyethylene glycol (molecular weight = 20 000; Sigma), and 0.5% Igepal CA-630 (Sigma) in PBS. After 30 minutes at 37 °C, color development was initiated by the addition of ABTS peroxidase solution (Kirkegaard and Perry, Gaithersburg, MD). The reaction was stopped after 20 minutes by adding 1% sodium dodecyl sulfate, and the optical density (OD) was measured at 405 nm, with a reference wavelength of 490 nm, in an automated microtiter plate reader (Molecular Devices, Menlo Park, CA). The cut point for seropositivity was determined from the reactivity of plasma samples from 108 women who were self-reported virgins from Costa Rica. The mean and standard deviation (SD) of optical density values for the control subjects were calculated, and values greater than the mean plus three standard deviations were excluded. The analysis was repeated on the remaining samples until no further optical density values could be excluded by this criterion. After four rounds of analysis, with the exclusion of six samples, the cutoff point was defined as five standard deviations above the mean of this distribution (0.187 U).
Determination of Antibodies Against HPV16 E6 and E7
Plasma antibodies against HPV16 E6 and E7 proteins were detected with an ELISA that used the glutathione S-transferase (GST) capture method with bacterially expressed full-length E6 or E7 fused to GST as the antigens, as described in detail previously (23). A preparatory experiment (Pawlita M: unpublished data) directly compared serum and plasma samples with and without heat inactivation for 30 minutes at 56 °C from 20 patients with cervical carcinoma and 20 healthy control subjects and found that heat inactivation and the use of plasma instead of serum did not alter ELISA reactivity with HPV16 E6 and E7 proteins or increase unspecific background.
In brief, 96-well Polysorb plastic plates (Nunc, Roskilde, Denmark) were coated with glutathione-casein. After blocking with unmodified casein (0.2% unmodified casein in PBS containing 0.05% Tween 20), plates were incubated with 100 μL of cleared lysate (diluted in casein-blocking buffer to a total lysate protein concentration of 0.25 μg/μL) from Escherichia coli overexpressing the antigen as a GST fusion protein or GST alone for background determination. Human plasma samples were heat inactivated and diluted 1 : 50 in blocking buffer containing total lysate protein from E. coli overexpressing GST without E6 or E7 sequences at 0.25 μg/μL. Bound human antibodies were detected by donkey anti-human IgG (heavy and light chain) polyclonal antibody, which recognizes all classes of human immunoglobulins, conjugated to horseradish peroxidase (Dianova, Hamburg, Germany). The absorbance from wells with GST alone defined the background reactivity of a human plasma and was subtracted from the absorbance of wells with the GST-E6 or GST-E7 proteins to calculate the specific reactivity of a sample with the respective antigen. Interassay variation ranged from 0.12 to 0.23. Each plasma sample was tested in duplicate on different plates. A mean specific reactivity of greater than 0.08 optical density units and a variation of the duplicate values of greater than 40% were set as cut points for repeat analysis, again in duplicates. Median optical density values were used for further analysis to reduce the impact of extreme outliers.
Cutoff determination for serum groups from individuals who did not have cancer from Germany, Tanzania, and Colombia (calculated as mean + 3 SDs, excluding positive outliers) yielded cutoff values for HPV16 E6 and E7 between 0.06 and 0.09 optical density units. To reduce the influence of borderline positive sera, a stringent cutoff point of 0.16 optical density units was arbitrarily defined for both HPV16 E6 and E7 ELISAs before analysis of the data.
Statistical Analysis
Cancers of the oropharynx and tonsil were combined as cancers of the oropharynx, and cancers at other sites were combined as cancers of the oral cavity. When multiple topographies were reported, tonsil and oropharynx were classified as oropharynx regardless of whether other locations were mentioned. Because of a report (24) that combined sites in the Waldeyer’s ring (oropharynx, tonsil, and base of the tongue), we considered adding base of the tongue to the oropharynx group, but the HPV markers in our specimens from patients with cancer of the base of the tongue were more similar to those from oral cavity cancers than to those from oropharynx cancers, and therefore we kept our original classification.
Odds ratios (ORs) and 95% confidence intervals (CIs) were computed for all centers combined by using unconditional multivariable logistic regression models. All models included terms for age, sex, country, smoking tobacco, paan chewing, and drinking alcohol, as appropriate.
For case patients and control subjects with available serologic biomarker data, the odds ratios were calculated as estimates of disease risk. For HPV DNA in biopsy specimens, we estimated the odds ratios of HPV detection in cancers of the oropharynx compared with cancers of the oral cavity. All models included terms for study design variables (i.e., age group, country, and sex) and, when appropriate, smoking tobacco, chewing tobacco, and drinking alcohol. The combined effect of HPV and smoking was assessed as a departure from a multiplicative logistic regression model. The method used to assess departure from a multiplicative model was the inclusion in the logistic regression models of an interaction term. Because of the different method used to select control subjects in India and the large number of subjects recruited in that country, we repeated the main analyses excluding the Indian centers and obtained similar results for all the analyses presented in the “Results” section.
Results
A total of 1670 case patients and 1732 control subjects were recruited (Table 1). Of the case patients, 1415 had cancers of the oral cavity and 255 had cancers of the oropharynx. Participation among case patients ranged from 76.5% in Spain to 99.0% in Cuba, for an overall participation rate of 88.7%; participation among control subjects ranged from 49.0% in Northern Ireland to 96.0% in Italy, for an overall participation rate of 87.3%. The proportion of the total case patients recruited in each center who had cancers of the oropharynx varied between 2.6% in Sudan and 41.7% in Italy. This difference did not reflect the actual proportion occurring in each location but did reflect the different referral patterns of the participating hospitals.
Biopsy specimens were available for 79.2% (1323) of case patients, of which 10% were not tested for HPV DNA because they contained only necrotic tissue. Valid PCR biopsy results (β-globin-positive) were available from 908 case patients (54.4% of those recruited). When case patients with valid PCR results were compared with case patients with missing results by using a multivariable logistic regression model, no statistically significant differences were found in age, sex, smoking, alcohol consumption and, in India, paan chewing habits (data not shown). However, case patients without valid PCR results were more likely to be from India, Cuba, Sudan, and Australia—the areas with the most challenging storage and transportation conditions.
HPV16 E6 and E7 serology results were available for 93.5% of case patients and 91.3% of control subjects. HPV16 L1 VLP serology results were available for 92.0% of case patients and 88.2% of control subjects. Exfoliated cells were obtained from more than 95% of case patients and control subjects, but testing was limited to 43.6% of these subjects, as discussed above. Cancer stage was ascertained for 1558 (93.3%) of participating case patients and was distributed as follows: stage I, 14.7%; stage II, 18.6%; stage III, 29.1%; and stage IV, 37.4%.
The distribution of case patients and control subjects by selected risk factors and odds ratios associated with selected variables is shown in Table 2. As expected, smoking was a strong risk factor for cancer of the oral cavity and, most notably, cancer of the oropharynx, with a clear dose-response relationship between cancer risk and increasing number of cigarettes smoked per day. A clear dose-response relationship between risk for cancer and the number of years of smoking was also found (data not shown). Similarly, number of alcoholic drinks per day (Table 2) and duration of alcohol drinking (data not shown) were associated with a dose-dependent increase in risk. Paan chewing, which could be evaluated only in India, was associated with a strong dose-dependent increase in the risk for cancer of the oral cavity. We did not observe an association between sexual behavior indicators, such as lifetime number of sexual partners and the practice of oral sex, and overall risk for cancer of the oral cavity or oropharynx.
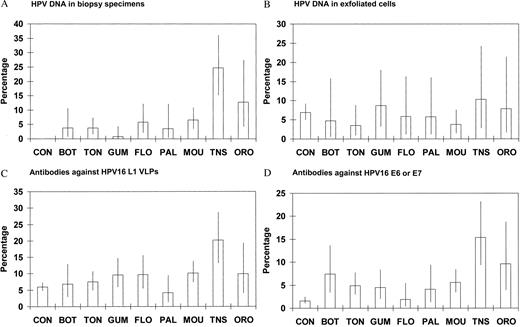
The prevalence of the different HPV markers (HPV DNA in biopsy specimens from cancer patients, HPV DNA in cells, and antibodies against HPV16 L1, E6, and E7 from case patients and control subjects) by topographic site of the primary tumor is shown in Fig. 1. The tonsil was the site with the highest prevalence of all markers, followed in most instances by the oropharynx. Control subjects had among the lowest positivities for most markers, except HPV DNA in exfoliated cells, which was somewhat more common in control subjects than in case patients with tumors of several oral cavity sites.
The association of various HPV markers with risk for cancer of the oral cavity and oropharynx, determined in a multivariable model, is shown in Table 3. HPV DNA was detected in biopsy specimens of 3.9% (95% CI = 2.5% to 5.3%) of cancers of the oral cavity (30 of 766 specimens with valid PCR results) and in biopsy specimens of 18.3% (95% CI = 12.0% to 24.7%) of cancers of the oropharynx (26 of 142 specimens with valid PCR results) (case-case comparison for cancers of the oropharynx/cancers of the oral cavity: OR = 4.9, 95% CI = 2.6 to 9.1). HPV16 was the only HPV type found in biopsies of 89.3% of HPV DNA-positive case patients, and HPV16 was present with HPV18 in an additional 5.4%, for a total of 94.7% HPV16 among positive case patients (data not shown). One case patient had HPV18 alone, one had HPV33 and HPV35, and one had HPV35 alone.
In multivariable models, after adjustment for age, sex, country, drinking alcohol, smoking tobacco, and chewing tobacco, as appropriate, detection of HPV DNA in tumors was not statistically significantly different by age, sex, country, or alcohol use (data not shown). However, HPV DNA was detected less frequently in biopsy specimens from ex-smokers (OR for detection of HPV DNA = 0.6, 95% CI = 0.2 to 1.5) and current smokers (OR = 0.4, 95% CI = 0.2 to 0.9) than in biopsy specimens from nonsmokers. In India, HPV DNA was detected less frequently in tumor specimens from tobacco chewers (OR for HPV detection = 0.5, 95% CI = 0.1 to 2.0) than in those from non-chewers. Case patients reporting more than one sexual partner in their lifetime were more likely to have HPV DNA in their tumors than those reporting only one sexual partner (OR for HPV detection = 2.4, 95% CI = 1.0 to 5.7), as were those reporting a history of oral sex compared with those without such a history (OR for HPV detection = 3.2, 95% CI = 1.5 to 6.4). The association of HPV DNA with sexual behavior was similar for cancers of the oral cavity and oropharynx, although some of the estimates were not statistically significant (data not shown).
The prevalence of HPV DNA detected in exfoliated cells was 4.7% (95% CI = 2.9% to 6.5%) for patients with cancer of the oral cavity, 8.9% (95% CI = 3.0% to 14.8%) for patients with cancer of the oropharynx, and 6.9% (95% CI = 4.9% to 8.9%) for control subjects (confidence intervals for prevalence not shown in tables). No statistically significant association between HPV DNA and risk for either type of cancer was noted in the case-control comparisons. In the case-case comparison, the odds ratio for HPV DNA positivity in cells was 2.0 (95% CI = 0.7 to 5.1) for cancers of the oropharynx compared with that for cancer of the oral cavity.
Antibodies against HPV16 L1 were detected in plasma from 6.0% of control subjects, 8.9% of case patients with cancers of the oral cavity (OR = 1.5, 95% CI = 1.1 to 2.1), and 13.4% of case patients with cancers of the oropharynx (OR = 3.5, 95% CI = 2.1 to 5.9). A statistically significant association between antibodies against HPV16 L1 and risk was also found in case-case comparisons (OR = 1.9, 95% CI = 1.2 to 3.0) for cancer of the oropharynx compared with cancer of the oral cavity.
Antibodies against HPV16 E6 were detected in 1.1% of control subjects, 2.6% of cancers of the oral cavity (OR = 2.6, 95% CI = 1.4 to 5.0), and 9.9% of cancers of the oropharynx (OR = 9.9, 95% CI = 4.7 to 20.7). A statistically significant association between HPV16 E6 and risk was also found in case-case comparisons (OR = 4.4, 95% CI = 2.3 to 8.2) for cancer of the oropharynx compared with cancer of the oral cavity, similar to that for HPV DNA in biopsy specimens. Similar patterns were observed for antibodies against HPV16 E7 (Table 3). Thus, antibodies against either HPV16 E6 or E7 or both were associated with the risk for cancers of the oral cavity (OR = 2.9, 95% CI = 1.7 to 4.8) and the oropharynx (OR = 9.2, 95% CI = 4.8 to 17.7).
Among control subjects, we found no statistically significant association between HPV immunologic biomarkers (antibodies against HPV16 L1, E6, or E7) and age, sex, smoking, drinking, or sexual behavior (data not shown). Prevalence of HPV16 L1 antibodies among control subjects varied between countries from 0% in Ireland, Poland, and Canada to 10.5% in Cuba; antibodies against HPV16 E6 or E7 were found infrequently in the same countries where HPV16 L1 antibodies were infrequent and were most frequently found among control subjects in Australia (10.5%, n = 60).
Antibodies against both HPV16 E6 and E7 were rarely detected in control subjects (0.1% of control subjects or 7.7% of those with detectable antibodies against HPV16 E6 or E7) and in case patients with cancers of the oral cavity (0.5% [9.8% of positive specimens]) but were more common in case patients with cancers of the oropharynx (6.6% [55.2% of positive specimens]). A strong association between detection of both HPV16 E6 and E7 antibodies and risk for cancer of the oropharynx was found (OR = 67.1, 95% CI = 12.9 to 348.2). Accordingly, a strong association was detected in the case-case comparison for cancer of the oropharynx compared with cancer of the oral cavity (OR = 13.5, 95% CI = 4.4 to 41.1). These associations were similar in both sexes, in different regions, and in two age strata (<60 years old and ≥60 years old).
HPV DNA was detected at a higher level in stages III–IV cancers of the oropharynx (21.5%) than in stages 0–II (7.4%) (P = .09). Antibodies against HPV16 E6 or E7 were also more commonly detected in specimens from more advanced stage cancers of the oropharynx than in specimens from earlier stage cancers of the oropharynx (14.7% of the 184 case patients at stages III–IV versus 2.4% for the 41 case patients at stages 0–II; P = .03), but antibodies against HPV16 E6 or E7 did not vary by stage of cancer of the oral cavity (data not shown). Antibodies against HPV16 L1 did not vary with the stage of either cancer examined in this study.
We next analyzed how frequently antibodies against HPV16 L1, E6, and E7 were detected in case patients with biopsy specimens in which HPV DNA was or was not detected (Table 4). Antibodies against HPV16 L1, E6, and E7 were more common in case patients whose biopsy specimens were positive for HPV DNA than in those whose biopsy specimens were negative for HPV DNA. This association was particularly strong for cancers of the oropharynx, in which HPV16 L1 antibodies were present in 52% and HPV16 E6 or E7 antibodies were present in 65.4% of case patients with biopsies positive for HPV DNA. In case patients with cancer of the oral cavity, there was very little correlation between detection of HPV16 DNA in biopsies and detection of HPV16 E6 or E7 antibodies (κ = 0.080, 95% CI = 0.001 to 0.226). For cancer of the oropharynx, the correlation was much stronger (κ = 0.6, 95% CI = 0.4 to 0.8). Corresponding sensitivities (using DNA in biopsy specimens as the gold standard) were 14% (95% CI = 4.7% to 31.9%) for oral cavity and 64% (95% CI = 46.5% to 77.1%) for oropharynx, with specificities close to 95% for both.
Little correlation was observed between the detection of HPV DNA in exfoliated cells and the detection of HPV DNA in biopsy specimens for the limited number of subjects (n = 349) who had both measurements (κ = 0.059, 95% CI = −0.035 to 0.281; Table 5). Ninety percent of the patients with biopsy specimens that were positive for HPV DNA had exfoliated cells in which HPV DNA was not detected.
Associations between cancer and the combined presence of HPV16 L1 VLP antibodies and a history of smoking and/or chewing tobacco are shown in Table 6. When compared with never smokers and/or never chewers who were negative for HPV16 L1 VLP, smokers who were negative for HPV16 L1 VLP (OR = 6.6, 95% CI = 5.3 to 8.2) and, to a lesser extent, never smokers who were positive for HPV16 L1 VLP (OR = 1.3, 95% CI = 0.7 to 2.3), and smokers who were positive for HPV16 L1 VLP (OR = 11.4, 95% CI = 7.4 to 17.6) had an increased risk for cancer of the oral cavity (P for departure from multiplicative model = .461). When compared with never smokers who were negative for HPV16 L1 VLP, smokers who were negative for HPV16 L1 VLP (OR = 9.2, 95% CI = 4.9 to 17.1), never smokers who were positive for HPV16 L1 VLP (OR = 6.7, 95% CI = 2.3 to 19.1), and smokers who were positive for HPV16 L1 VLP (OR = 26.6, 95% CI = 11.9 to 59.4) had an increased risk for cancers of the oropharynx (P for departure from multiplicative model = .181).
Associations between the risk for cancer and the combined presence of HPV16 E6 or E7 antibodies and a history of tobacco smoking and/or paan chewing are also shown in Table 6. When compared with never smokers/never chewers who were negative for HPV16 E6 and E7, smokers/chewers who were negative for HPV16 E6 and E7 (OR = 6.7, 95% CI = 5.4 to 8.4), never smokers/never chewers who were positive for HPV16 E6 or E7 (OR = 6.7, 95% CI = 2.6 to 17.3), and smokers who were positive for HPV16 E6 or E7 (OR = 13.0, 95% CI = 7.2 to 23.5) had an increased risk for cancer of the oral cavity. The odds ratio for cancer of the oral cavity for HPV-positive smokers was much lower than that expected under a multiplicative model (P for departure from multiplicative model = .03), in a typical pattern for an additive effect. When compared with never smokers who were negative for HPV16 E6 and E7, smokers who were negative for HPV16 E6 and E7 (OR = 11.2, 95% CI = 5.9 to 21.4), never smokers who were positive for HPV16 E6 or E7 (OR = 64.5, 95% CI = 18.3 to 226.7), and smokers who were positive for HPV16 E6 or E7 (OR = 56.2, 95% CI = 22.5 to 140.4) had an increased risk for cancer of the oropharynx. The odds ratio for HPV-positive smokers was again much lower than that expected under a multiplicative model (P for departure from multiplicative model = .001), in a pattern typical of an additive effect.
Discussion
This large case-control study evaluated the association between five markers of HPV infection and cancers of the oral cavity and the oropharynx (HPV DNA in biopsy specimens, HPV DNA in exfoliated cells, and antibodies against HPV16 L1, E6, and E7). We recruited more than 1600 case patients and 1700 control subjects in nine countries and used similar protocols for data and specimen collection and centralized HPV testing. Our results indicate that HPV appears to play a definite etiologic role in a substantial fraction of cancers of the oropharynx and possibly in a small subgroup of cancers of the oral cavity. Nonsmokers are more likely than smokers to have HPV-related tumors.
HPV DNA was detected in tumor biopsy specimens from 18.3% of case patients with cancer of the oropharynx and from 3.9% of patients with cancer of the oral cavity, which is an adjusted fivefold increase in the odds of HPV detection in case patients with cancer of the oropharynx compared with that in case patients with cancer of the oral cavity. Among the topographic sites examined, HPV was most frequently detected in cancer of the tonsil (24.7% of specimens). These prevalences are consistent with, albeit somewhat lower than, those in previous reports [for review, see (2,25)]. Similar to the results of other studies (9–11), the vast majority (95%) of HPV-positive case patients in this study had HPV16, the most common type in genital cancers. The exclusive detection of HPV DNA by PCR may, however, lead to overestimation of the number of case patients in which the virus is etiologically involved, as suggested by the lower proportion of case patients in whom HPV16 E6 and/or E7 antibodies could also be detected.
As reported by Gillison et al. (9), we detected HPV DNA statistically significantly less often among tobacco smokers and/or chewers than among nonsmokers and/or non-chewers. HPV was detected more commonly in biopsy specimens from cancer patients with more than one sexual partner and from those who practiced oral sex than in biopsy specimens from those with fewer than two partners or who did not engage in oral sex, suggesting the possibility of sexual transmission. Schwartz et al. (11) also found an association between sexual behavior and risk for HPV16-positive cancers for both sexes combined. However, much remains to be learned about the transmission of HPV in normal subjects and the natural history of HPV infection in the oral cavity (14).
A relatively high percentage (24.2%) of case patients who were tested by PCR had invalid results because of the absence of adequate material (i.e., they were β-globin-negative). This problem was more common in case patients from India, Sudan, Cuba, and Australia, probably as a consequence of difficulties with storing and shipping specimens. However, case patients with valid results and without such results did not differ substantially in their risk factor profile.
HPV DNA in exfoliated cells was not detected more frequently in case patients than in control subjects. The poor association between HPV DNA test results from exfoliated cells and those from biopsy specimens probably indicates that the HPV status of exfoliated cells does not accurately reflect that of tumors. HPV was not detected in exfoliated cells from 90% of the case patients with HPV-positive biopsy specimens. This result is in concordance with those of Schwartz et al. (11), although their specimens were collected after treatment. In contrast, Smith et al. (10) detected a threefold increased risk for oral cavity and oropharyngeal cancer associated with the detection of HPV DNA in exfoliated cells before treatment. Thus, the appropriate marker of HPV exposure measurable in case patients and control subjects remains elusive, particularly given the biologic diversity of individual topographic sites in the oral cavity (14).
Using several different HPV markers (HPV DNA in biopsy specimens, HPV DNA in exfoliated cells, and antibodies against HPV16 L1, E6, and E7), we found a strong association between HPV and cancer of the oropharynx and also some association between HPV and cancer of the oral cavity. The latter association could be partly explained by misclassification of the tumor site if some HPV-positive cancers of the oropharynx were classified erroneously as cancers of the oral cavity, but it could also indicate that a small fraction of oral cavity lesions are HPV-related.
Although antibodies against HPV16 L1 are relatively insensitive markers of cumulative exposure to the virus, such antibodies were associated with a 1.5-fold increased risk for cancer of the oral cavity and a 3.5-fold increased risk for cancer of the oropharynx, with a 2-fold increased risk for cancer of the oropharynx compared with that of the oral cavity. In a recent prospective study (13), a twofold increased risk was observed for head and neck tumors in subjects with detectable antibodies against HPV16 L1 or L2 proteins and, similar to our findings, risk was highest for cancer of the tonsil and oropharynx with a smaller increased risk for cancer of the tongue. Although there was some degree of adjustment for smoking by the use of cotinine levels in that study (13), the authors could not account for other confounding factors. Schwartz et al. (11) also investigated the association of antibodies against L1 with oral cancer and detected a twofold increased risk for all tumors and an almost sevenfold increased risk for HPV16-positive cancers. When interpreting associations between the risk for cancer and the presence of these antibodies, it should be noted that they reflect infection in all susceptible mucosal sites, which may introduce additional sources of confounding. Moreover, not all individuals exposed to HPV seroconvert or maintain detectable antibody levels over time.
HPV16 E6 and E7 antibodies are generally considered markers of invasive HPV16-transformed tumors, possibly generated after antigen exposure, after development of a tumor vascular bed, or after necrosis has occurred (26,27). A recent prospective study (28) conducted to evaluate the predictive value of E6 and E7 antibodies as markers of early cervical cancer demonstrated that only 7% of women who developed cervical cancer in the 0.5–20 years after blood was drawn had detectable levels of E6 or E7 antibodies and had a modest increased risk for later developing cervical cancer compared with women without such antibodies. However, some degree of expression of these oncoproteins is probably present also in HPV infections and dysplastic lesions. In fact, a recent study (29) reported relatively high prevalence of these antibodies in patients with evidence of HPV infection but not cervical cancer. It can be argued that if these antibodies are markers of invasion, their use as markers of exposure in control subjects may overestimate the risk. However, such antibodies can be detected in a few control subjects, and they can be helpful in identifying HPV-related cancers in tumor sites with heterogeneous etiologies. In our study, these antibodies were strongly associated with cancer of the oropharynx, with odds ratios near 10 for antibodies against HPV16 E6, 20 for antibodies against HPV16 E7, and almost 70 for the combination of the two. Conversely, risk for cancer of the oral cavity was increased about threefold when HPV16 E6 or E7 antibodies were detected, and it was not much higher when both were detected.
A high prevalence of anti-HPV16 E6 and E7 antibodies is observed in advanced cervical cancer (30). In our study, 65% of case patients with HPV16 DNA-positive cancers of the oropharynx had antibodies against HPV16 E6 or E7, making these proteins potentially useful and minimally invasive markers of HPV-related tumors when appropriate cytologic or histologic specimens are not available. The lower antibody prevalence in HPV DNA-positive cancers of the oral cavity than in cancers of the oropharynx might indicate a noncausal association between HPV and cancer of the oral cavity, or it may reflect lower viral oncogene expression, less invasive growth, or as yet unidentified site-dependent differences in antibody response to the HPV oncoproteins.
Given that the different HPV markers are probably measuring different aspects of HPV infection and that each has different sampling and technical limitations, none of these risk estimates can ultimately quantify the association between HPV and cancer of the oral cavity or oropharynx. The strength of our findings is the consistency in the direction of the associations with all the markers, which were measured independently by investigators masked to case-control status, topography, and other variables.
We investigated the combined effect of tobacco use and HPV infection by using antibodies against HPV16 L1 VLPs and antibodies against HPV16 E6 and E7. For the latter, the risks appeared to be additive, indicating the absence of synergism between tobacco use and HPV. The exclusion of case patients from India only strengthened the additivity of the effects of tobacco and HPV (data not shown). Schwartz et al. (11) detected a synergistic (i.e., multiplicative) effect of smoking and HPV, as measured by antibodies against HPV16 L1 VLPs. In our study, the combined effects of HPV16 L1 VLP antibodies and smoking did not show a statistically significant departure from the multiplicative model. However, small numbers may have hampered our ability to clarify the type of interaction, because we could not restrict the analysis to heavy smokers. The presence of additive rather than multiplicative risks between HPV and smoking/chewing tobacco use would suggest that these factors operate, in part, at the same step of multistage carcinogenesis in the oral cavity and oropharynx (e.g., p53 inactivation). Still, HPV infection appears to contribute to an increased risk for cancer of the oral cavity and oropharynx also among tobacco smokers and chewers.
In addition to mounting epidemiologic evidence, extensive laboratory evidence (14) supports the association between HPV and a subset of cancers of the oropharynx. HPV16 E6 protein inactivates p53 protein, and HPV-associated tumors of the cervix and other anogenital sites [for review, see(31)] do not usually have TP53 mutations. Tumors at those locations that contain HPV DNA contain TP53 mutations less frequently than HPV-negative tumors, and tumors that express HPV16 E6 or E7 usually do not have a mutated TP53 gene (32,33). HPV-associated cancers of the oral cavity and oropharynx are more likely to have basaloid histologic features (9,33), an aspect we did not evaluate. Viral E6 and/or E7 transcripts and/or viral integration have been detected more frequently in tumors containing HPV16 or HPV33 DNA (34,35), and both in situ hybridization studies and microdissection studies have detected viral DNA or RNA in the tumor but not in the stroma (36). In addition, a cell line with integrated HPV16 was established from an HPV16-containing oral carcinoma (37). Thus, the laboratory and epidemiologic data indicate that HPV may be a causal factor in a subset of oral and oropharyngeal carcinomas and may operate through the same mechanisms described in the pathogenesis of all cervical carcinomas.
A parallel among oral, vulvar, vaginal, penile, and anal cancers is apparent in that only a fraction of tumors at these sites appear to be related to HPV (8). Strong risk factors other than HPV exist for cancers of the oral cavity and oropharynx; therefore, the relative contribution of HPV would probably be larger in regions where exposures such as tobacco smoking and chewing are less common, although cancers of the oral cavity and oropharynx would be rare. The mechanism of transmission of HPV to the oral cavity warrants further investigation. The prospect of HPV vaccine development (38) offers hope for prevention of cervical and anogenital cancers and possibly also for a substantial number of cancers of the oropharynx and oral cavity.
Appendix
In addition to the authors of this article, the following investigators are part of the IARC Multicenter Oral Cancer Study Group and they participated in this study: Rengaswamy Sankaranarayanam, IARC, Lyon, France; Eduardo Franco, McGill University, Montreal, Quebec, Canada; Parviz Ghadirian, Université de Montréal, Montreal; Carmen Martinez, Escuela Andaluza de Salud Publica, Granada, Spain; Angel Rollón, Jose Ramón Armas, Hospital Virgen Macarena, Seville, Spain; Philip Lamey, Ruth Leathem, Queen’s University Belfast, Northern Ireland, United Kingdom; Juan Lence, Rosa Maria Ortiz, Teresa Cruz, María de los Angeles Ríos, Instituto Nacional de Oncologia y Radiobiologia, Havana, Cuba; Maria Jesús Quintana, Miquel Quer, Hospital de Sant Pau, Barcelona, Spain; Antoni Monner, Amparo Juan, Marta Carrera, Ciutat Sanitària i Universitària de Bellvitge, Bellvitge, Spain; Gina Albero, Institut Català d’Oncologia, Barcelona, Spain; Paul van der Valk, Vrije Universiteit Medical Center, Amsterdam, The Netherlands; Kamal H. Mohamed, Toombak and Smoking Research Center, Khartoum, Sudan; Juan Ramon Delgado, Adoración Martínez, Hospital Virgen de las Nieves, Granada, Spain; Peter Sehr, Deutsches Krebsforschungszentrum, Heidelberg, Germany; Janusz Piekarczyk, Danuta Samolczyk-Wanyura, Agnieszka Pilarska, Pawel Pilarski, 2nd, Maxillofacial Surgery Clinic, Medical Academy, and Witold Zatonski, Cancer Center, Warsaw, Poland; Christopher O’Brien, Sydney Head and Neck Cancer Institute, Royal Prince Alfred Hospital, Sydney, Australia; Silvana Pilotti, Istituto Nazionale per la Cura e lo Studio dei Tumori, Milan, Italy; Rudrapatna Jayshree Subramanyam, Sakaleshpur Veerappaiah Kumaraswamy, Geetashree Mukherjee, Kidwai Memorial Institute of Oncology, Bangalore, India.
Prevalence of human papillomavirus (HPV) markers among control subjects and by cancer subsite. CON = control subjects; BOT = base of the tongue; TON = other parts of the tongue; GUM = gum; FLO = floor of the mouth; PAL = palate; MOU = mouth; TNS = tonsil; ORO = oropharynx. Bars indicate 95% confidence intervals. Estimates presented for each of the markers are based on all subjects tested for that marker. The number of subjects tested was particularly limited for HPV DNA in cells. A) Prevalence of HPV DNA detection in biopsy specimens by cancer subsite (specimens not available from control subjects). B) Prevalence of HPV DNA detection in exfoliated cells among control subjects and by cancer subsite. C) Prevalence of antibodies against HPV16 L1 virus-like particles among control subjects and by cancer subsite. D) Prevalence of antibodies against HPV16 E6 or E7 among control subjects and by cancer subsite.
Distribution of study participants by country and availability of various markers of human papillomavirus (HPV) infection*
| Country . | % participation . | No. recruited . | . | . | Biopsy specimens . | . | HPV serology . | . | Cells . | . | . | Valid PCR results No. (%) . | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| . | . | Control . | OC . | OP . | No. obtained . | No. PCR-tested . | Valid PCR results, No. (%) . | E6/E7 results, No. (%) . | L1 results, No. (%) . | No. obtained . | No. PCR-tested . | . | ||||||||||||
| Case patients | ||||||||||||||||||||||||
| Italy | 92.0 | 77 | 55 | 106 | 101 | 89 (67.4) | 129 (97.7) | 129 (97.7) | 131 | 46 | 42 (31.8) | |||||||||||||
| Spain | 76.5 | 287 | 72 | 265 | 243 | 216 (60.2) | 333 (92.8) | 331 (92.2) | 338 | 145 | 140 (39.0) | |||||||||||||
| Northern Ireland | 85.0 | 60 | 10 | 38 | 35 | 32 (45.7) | 61 (87.1) | 61 (87.1) | 69 | 29 | 29 (41.4) | |||||||||||||
| Poland | 96.0 | 113 | 8 | 113 | 102 | 90 (74.4) | 101 (83.5) | 102 (84.3) | 121 | — | — | |||||||||||||
| India | 93.0 | 547 | 35 | 438 | 398 | 274 (47.1) | 572 (98.3) | 572 (98.3) | 565 | 460 | 329 (56.5) | |||||||||||||
| Cuba | 99.0 | 150 | 47 | 174 | 154 | 104 (52.8) | 190 (96.4) | 185 (93.9) | 191 | 31 | 29 (14.7) | |||||||||||||
| Canada | 82.6 | 43 | 14 | 57 | 40 | 35 (61.4) | 49 (86.0) | 43 (75.4) | 57 | — | — | |||||||||||||
| Australia | 96.0 | 26 | 11 | 37 | 36 | 24 (64.9) | 33 (89.2) | 20 (54.1) | 36 | — | — | |||||||||||||
| Sudan | NA | 112 | 3 | 95 | 89 | 44 (38.3) | 94 (81.7) | 94 (81.7) | 102 | 45 | 32 (27.8) | |||||||||||||
| Total | 88.7 | 1415 | 255 | 1323 | 1198 | 908 (54.4) | 1562 (93.5) | 1537 (92.0) | 1610 | 756 | 601 (36.0) | |||||||||||||
| Control subjects | ||||||||||||||||||||||||
| Italy | 96.0 | 148 | 146 (98.6) | 146 (98.6) | 148 | 51 | 47 (31.8) | |||||||||||||||||
| Spain | 91.0 | 375 | 303 (80.8) | 301 (80.3) | 367 | 117 | 114 (30.4) | |||||||||||||||||
| Northern Ireland | 49.0 | 50 | 50 (100.0) | 50 (100.0) | 50 | 15 | 15 (30.0) | |||||||||||||||||
| Poland | 93.0 | 124 | 112 (90.3) | 104 (83.9) | 123 | — | — | |||||||||||||||||
| India | 90.0 | 582 | 564 (96.9) | 563 (96.7) | 576 | 410 | 364 (62.5) | |||||||||||||||||
| Cuba | 81.0 | 200 | 196 (98.0) | 191 (95.5) | 196 | 23 | 23 (11.5) | |||||||||||||||||
| Canada | 82.2 | 42 | 42 (100.0) | 41 (97.6) | 42 | — | — | |||||||||||||||||
| Australia | 94.0 | 60 | 38 (63.3) | 6 (10.0) | 59 | — | — | |||||||||||||||||
| Sudan | NA | 151 | 130 (86.1) | 125 (82.8) | 98 | 52 | 50 (33.1) | |||||||||||||||||
| Total | 87.3 | 1732 | 1581 (91.3) | 1527 (88.2) | 1659 | 668 | 613 (35.4) | |||||||||||||||||
| Country . | % participation . | No. recruited . | . | . | Biopsy specimens . | . | HPV serology . | . | Cells . | . | . | Valid PCR results No. (%) . | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| . | . | Control . | OC . | OP . | No. obtained . | No. PCR-tested . | Valid PCR results, No. (%) . | E6/E7 results, No. (%) . | L1 results, No. (%) . | No. obtained . | No. PCR-tested . | . | ||||||||||||
| Case patients | ||||||||||||||||||||||||
| Italy | 92.0 | 77 | 55 | 106 | 101 | 89 (67.4) | 129 (97.7) | 129 (97.7) | 131 | 46 | 42 (31.8) | |||||||||||||
| Spain | 76.5 | 287 | 72 | 265 | 243 | 216 (60.2) | 333 (92.8) | 331 (92.2) | 338 | 145 | 140 (39.0) | |||||||||||||
| Northern Ireland | 85.0 | 60 | 10 | 38 | 35 | 32 (45.7) | 61 (87.1) | 61 (87.1) | 69 | 29 | 29 (41.4) | |||||||||||||
| Poland | 96.0 | 113 | 8 | 113 | 102 | 90 (74.4) | 101 (83.5) | 102 (84.3) | 121 | — | — | |||||||||||||
| India | 93.0 | 547 | 35 | 438 | 398 | 274 (47.1) | 572 (98.3) | 572 (98.3) | 565 | 460 | 329 (56.5) | |||||||||||||
| Cuba | 99.0 | 150 | 47 | 174 | 154 | 104 (52.8) | 190 (96.4) | 185 (93.9) | 191 | 31 | 29 (14.7) | |||||||||||||
| Canada | 82.6 | 43 | 14 | 57 | 40 | 35 (61.4) | 49 (86.0) | 43 (75.4) | 57 | — | — | |||||||||||||
| Australia | 96.0 | 26 | 11 | 37 | 36 | 24 (64.9) | 33 (89.2) | 20 (54.1) | 36 | — | — | |||||||||||||
| Sudan | NA | 112 | 3 | 95 | 89 | 44 (38.3) | 94 (81.7) | 94 (81.7) | 102 | 45 | 32 (27.8) | |||||||||||||
| Total | 88.7 | 1415 | 255 | 1323 | 1198 | 908 (54.4) | 1562 (93.5) | 1537 (92.0) | 1610 | 756 | 601 (36.0) | |||||||||||||
| Control subjects | ||||||||||||||||||||||||
| Italy | 96.0 | 148 | 146 (98.6) | 146 (98.6) | 148 | 51 | 47 (31.8) | |||||||||||||||||
| Spain | 91.0 | 375 | 303 (80.8) | 301 (80.3) | 367 | 117 | 114 (30.4) | |||||||||||||||||
| Northern Ireland | 49.0 | 50 | 50 (100.0) | 50 (100.0) | 50 | 15 | 15 (30.0) | |||||||||||||||||
| Poland | 93.0 | 124 | 112 (90.3) | 104 (83.9) | 123 | — | — | |||||||||||||||||
| India | 90.0 | 582 | 564 (96.9) | 563 (96.7) | 576 | 410 | 364 (62.5) | |||||||||||||||||
| Cuba | 81.0 | 200 | 196 (98.0) | 191 (95.5) | 196 | 23 | 23 (11.5) | |||||||||||||||||
| Canada | 82.2 | 42 | 42 (100.0) | 41 (97.6) | 42 | — | — | |||||||||||||||||
| Australia | 94.0 | 60 | 38 (63.3) | 6 (10.0) | 59 | — | — | |||||||||||||||||
| Sudan | NA | 151 | 130 (86.1) | 125 (82.8) | 98 | 52 | 50 (33.1) | |||||||||||||||||
| Total | 87.3 | 1732 | 1581 (91.3) | 1527 (88.2) | 1659 | 668 | 613 (35.4) | |||||||||||||||||
OC = cancer of the oral cavity; OP = cancer of the oropharynx; PCR = polymerase chain reaction; — = zero; NA = not ascertained.
Distribution of study participants by country and availability of various markers of human papillomavirus (HPV) infection*
| Country . | % participation . | No. recruited . | . | . | Biopsy specimens . | . | HPV serology . | . | Cells . | . | . | Valid PCR results No. (%) . | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| . | . | Control . | OC . | OP . | No. obtained . | No. PCR-tested . | Valid PCR results, No. (%) . | E6/E7 results, No. (%) . | L1 results, No. (%) . | No. obtained . | No. PCR-tested . | . | ||||||||||||
| Case patients | ||||||||||||||||||||||||
| Italy | 92.0 | 77 | 55 | 106 | 101 | 89 (67.4) | 129 (97.7) | 129 (97.7) | 131 | 46 | 42 (31.8) | |||||||||||||
| Spain | 76.5 | 287 | 72 | 265 | 243 | 216 (60.2) | 333 (92.8) | 331 (92.2) | 338 | 145 | 140 (39.0) | |||||||||||||
| Northern Ireland | 85.0 | 60 | 10 | 38 | 35 | 32 (45.7) | 61 (87.1) | 61 (87.1) | 69 | 29 | 29 (41.4) | |||||||||||||
| Poland | 96.0 | 113 | 8 | 113 | 102 | 90 (74.4) | 101 (83.5) | 102 (84.3) | 121 | — | — | |||||||||||||
| India | 93.0 | 547 | 35 | 438 | 398 | 274 (47.1) | 572 (98.3) | 572 (98.3) | 565 | 460 | 329 (56.5) | |||||||||||||
| Cuba | 99.0 | 150 | 47 | 174 | 154 | 104 (52.8) | 190 (96.4) | 185 (93.9) | 191 | 31 | 29 (14.7) | |||||||||||||
| Canada | 82.6 | 43 | 14 | 57 | 40 | 35 (61.4) | 49 (86.0) | 43 (75.4) | 57 | — | — | |||||||||||||
| Australia | 96.0 | 26 | 11 | 37 | 36 | 24 (64.9) | 33 (89.2) | 20 (54.1) | 36 | — | — | |||||||||||||
| Sudan | NA | 112 | 3 | 95 | 89 | 44 (38.3) | 94 (81.7) | 94 (81.7) | 102 | 45 | 32 (27.8) | |||||||||||||
| Total | 88.7 | 1415 | 255 | 1323 | 1198 | 908 (54.4) | 1562 (93.5) | 1537 (92.0) | 1610 | 756 | 601 (36.0) | |||||||||||||
| Control subjects | ||||||||||||||||||||||||
| Italy | 96.0 | 148 | 146 (98.6) | 146 (98.6) | 148 | 51 | 47 (31.8) | |||||||||||||||||
| Spain | 91.0 | 375 | 303 (80.8) | 301 (80.3) | 367 | 117 | 114 (30.4) | |||||||||||||||||
| Northern Ireland | 49.0 | 50 | 50 (100.0) | 50 (100.0) | 50 | 15 | 15 (30.0) | |||||||||||||||||
| Poland | 93.0 | 124 | 112 (90.3) | 104 (83.9) | 123 | — | — | |||||||||||||||||
| India | 90.0 | 582 | 564 (96.9) | 563 (96.7) | 576 | 410 | 364 (62.5) | |||||||||||||||||
| Cuba | 81.0 | 200 | 196 (98.0) | 191 (95.5) | 196 | 23 | 23 (11.5) | |||||||||||||||||
| Canada | 82.2 | 42 | 42 (100.0) | 41 (97.6) | 42 | — | — | |||||||||||||||||
| Australia | 94.0 | 60 | 38 (63.3) | 6 (10.0) | 59 | — | — | |||||||||||||||||
| Sudan | NA | 151 | 130 (86.1) | 125 (82.8) | 98 | 52 | 50 (33.1) | |||||||||||||||||
| Total | 87.3 | 1732 | 1581 (91.3) | 1527 (88.2) | 1659 | 668 | 613 (35.4) | |||||||||||||||||
| Country . | % participation . | No. recruited . | . | . | Biopsy specimens . | . | HPV serology . | . | Cells . | . | . | Valid PCR results No. (%) . | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| . | . | Control . | OC . | OP . | No. obtained . | No. PCR-tested . | Valid PCR results, No. (%) . | E6/E7 results, No. (%) . | L1 results, No. (%) . | No. obtained . | No. PCR-tested . | . | ||||||||||||
| Case patients | ||||||||||||||||||||||||
| Italy | 92.0 | 77 | 55 | 106 | 101 | 89 (67.4) | 129 (97.7) | 129 (97.7) | 131 | 46 | 42 (31.8) | |||||||||||||
| Spain | 76.5 | 287 | 72 | 265 | 243 | 216 (60.2) | 333 (92.8) | 331 (92.2) | 338 | 145 | 140 (39.0) | |||||||||||||
| Northern Ireland | 85.0 | 60 | 10 | 38 | 35 | 32 (45.7) | 61 (87.1) | 61 (87.1) | 69 | 29 | 29 (41.4) | |||||||||||||
| Poland | 96.0 | 113 | 8 | 113 | 102 | 90 (74.4) | 101 (83.5) | 102 (84.3) | 121 | — | — | |||||||||||||
| India | 93.0 | 547 | 35 | 438 | 398 | 274 (47.1) | 572 (98.3) | 572 (98.3) | 565 | 460 | 329 (56.5) | |||||||||||||
| Cuba | 99.0 | 150 | 47 | 174 | 154 | 104 (52.8) | 190 (96.4) | 185 (93.9) | 191 | 31 | 29 (14.7) | |||||||||||||
| Canada | 82.6 | 43 | 14 | 57 | 40 | 35 (61.4) | 49 (86.0) | 43 (75.4) | 57 | — | — | |||||||||||||
| Australia | 96.0 | 26 | 11 | 37 | 36 | 24 (64.9) | 33 (89.2) | 20 (54.1) | 36 | — | — | |||||||||||||
| Sudan | NA | 112 | 3 | 95 | 89 | 44 (38.3) | 94 (81.7) | 94 (81.7) | 102 | 45 | 32 (27.8) | |||||||||||||
| Total | 88.7 | 1415 | 255 | 1323 | 1198 | 908 (54.4) | 1562 (93.5) | 1537 (92.0) | 1610 | 756 | 601 (36.0) | |||||||||||||
| Control subjects | ||||||||||||||||||||||||
| Italy | 96.0 | 148 | 146 (98.6) | 146 (98.6) | 148 | 51 | 47 (31.8) | |||||||||||||||||
| Spain | 91.0 | 375 | 303 (80.8) | 301 (80.3) | 367 | 117 | 114 (30.4) | |||||||||||||||||
| Northern Ireland | 49.0 | 50 | 50 (100.0) | 50 (100.0) | 50 | 15 | 15 (30.0) | |||||||||||||||||
| Poland | 93.0 | 124 | 112 (90.3) | 104 (83.9) | 123 | — | — | |||||||||||||||||
| India | 90.0 | 582 | 564 (96.9) | 563 (96.7) | 576 | 410 | 364 (62.5) | |||||||||||||||||
| Cuba | 81.0 | 200 | 196 (98.0) | 191 (95.5) | 196 | 23 | 23 (11.5) | |||||||||||||||||
| Canada | 82.2 | 42 | 42 (100.0) | 41 (97.6) | 42 | — | — | |||||||||||||||||
| Australia | 94.0 | 60 | 38 (63.3) | 6 (10.0) | 59 | — | — | |||||||||||||||||
| Sudan | NA | 151 | 130 (86.1) | 125 (82.8) | 98 | 52 | 50 (33.1) | |||||||||||||||||
| Total | 87.3 | 1732 | 1581 (91.3) | 1527 (88.2) | 1659 | 668 | 613 (35.4) | |||||||||||||||||
OC = cancer of the oral cavity; OP = cancer of the oropharynx; PCR = polymerase chain reaction; — = zero; NA = not ascertained.
Characteristics of case patients and control subjects and risks associated with tobacco smoking, paan chewing, alcohol drinking, and sexual behavior*
| Characteristic . | No. of control subjects (%) . | Case patients . | . | . | . | |||
|---|---|---|---|---|---|---|---|---|
| . | . | Cancer of the oral cavity . | . | Cancer of the oropharynx . | . | |||
| . | . | No. (%) . | OR† (95% CI) . | No. (%) . | OR† (95% CI) . | |||
| Sex | ||||||||
| Male | 1078 (62.2) | 880 (62.2) | 214 (83.9) | |||||
| Female | 654 (37.8) | 535 (37.8) | 41 (16.1) | |||||
| Age, y | ||||||||
| ≤44 | 342 (19.7) | 177 (12.5) | 26 (10.2) | |||||
| 45–54 | 417 (24.1) | 319 (22.5) | 59 (23.1) | |||||
| 55–64 | 485 (28.0) | 422 (29.8) | 90 (35.3) | |||||
| ≥65 | 488 (28.2) | 497 (35.1) | 80 (31.4) | |||||
| No. of cigarettes per day‡ | ||||||||
| Never | 891 (51.8) | 542 (38.5) | 1.0 (referent) | 23 (9.3) | 1.0 (referent) | |||
| 1–5 | 106 (6.2) | 71 (5.0) | 1.4 (0.9 to 2.0) | 8 (3.2) | 2.4 (1.0 to 5.7) | |||
| 6–10 | 161 (9.4) | 121 (8.6) | 1.9 (1.4 to 2.6) | 25 (10.1) | 4.9 (2.6 to 9.2) | |||
| 11–15 | 96 (5.6) | 93 (6.6) | 2.9 (2.0 to 4.1) | 25 (10.1) | 7.0 (3.6 to 13.4) | |||
| 16–20 | 186 (10.8) | 208 (14.8) | 3.7 (2.8 to 5.0) | 46 (18.6) | 6.9 (3.8 to 12.5) | |||
| 21–30 | 157 (9.1) | 207 (14.7) | 4.5 (3.3 to 6.1) | 62 (25.1) | 13.2 (7.4 to 23.6) | |||
| >30 | 124 (7.2) | 167 (11.9) | 4.7 (3.4 to 6.6) | 58 (23.5) | 15.6 (8.5 to 28.8) | |||
| No. of alcoholic drinks per day§ | ||||||||
| Never drinker | 590 (43.0) | 388 (35.3) | 1.0 (referent) | 38 (15.9) | 1.0 (referent) | |||
| ≤4 | 605 (44.1) | 438 (39.8) | 1.3 (1.0 to 1.6) | 87 (36.4) | 1.2 (0.7 to 1.9) | |||
| 5–6 | 54 (3.9) | 79 (7.2) | 2.7 (1.7 to 4.2) | 24 (10.0) | 2.8 (1.4 to 5.6) | |||
| 7–10 | 58 (4.2) | 87 (7.9) | 2.9 (1.9 to 4.5) | 41 (17.2) | 4.8 (2.5 to 9.2) | |||
| 11–15 | 31 (2.3) | 51 (4.6) | 3.6 (2.1 to 6.1) | 25 (10.5) | 6.1 (2.9 to 12.9) | |||
| >15 | 33 (2.4) | 57 (5.2) | 3.3 (2.0 to 5.5) | 24 (10.0) | 6.0 (2.9 to 12.3) | |||
| No. of paan chewing units per day‖ | ||||||||
| Never chewer | 483 (84.0) | 139 (25.7) | 1.0 (referent) | 27 (81.8) | 1.0 (referent) | |||
| 1–5 | 65 (11.3) | 242 (44.8) | 14.5 (10.1 to 20.7) | 3 (9.1) | 0.6 (0.2 to 2.1) | |||
| 6–10 | 19 (3.3) | 116 (21.5) | 25.8 (15.1 to 44.4) | 2 (6.1) | 2.0 (0.4 to 10.0) | |||
| >10 | 8 (1.4) | 43 (8.0) | 21.7 (9.7 to 48.5) | 1 (3.0) | 4.5 (0.5 to 43.7) | |||
| Lifetime No. of sexual partners¶ | ||||||||
| 0–1 | 936 (60.9) | 807 (63.0) | 1.0 (referent) | 82 (35.7) | 1.0 (referent) | |||
| 2–5 | 256 (16.6) | 235 (18.3) | 0.9 (0.7 to 1.2) | 54 (23.5) | 1.1 (0.7 to 1.7) | |||
| 6–10 | 119 (7.7) | 88 (6.9) | 0.7 (0.5 to 1.0) | 28 (12.2) | 1.0 (0.6 to 1.8) | |||
| 11–20 | 88 (5.7) | 75 (5.9) | 0.8 (0.5 to 1.2) | 26 (11.3) | 1.1 (0.6 to 2.0) | |||
| 21–50 | 90 (5.9) | 44 (3.4) | 0.5 (0.3 to 0.7) | 23 (10.0) | 1.2 (0.7 to 2.2) | |||
| 51–100 | 27 (1.8) | 11 (0.9) | 0.4 (0.2 to 0.8) | 7 (3.0) | 1.0 (0.4 to 2.5) | |||
| >100 | 22 (1.4) | 21 (1.6) | 0.8 (0.4 to 1.6) | 10 (4.3) | 1.6 (0.7 to 3.9) | |||
| Frequency of oral sex# | ||||||||
| No oral sex | 1063 (75.7) | 881 (78.0) | 1.0 (referent) | 141 (66.2) | 1.0 (referent) | |||
| Occasionally | 216 (15.4) | 143 (12.7) | 0.9 (0.7 to 1.1) | 46 (21.6) | 0.8 (0.5 to 1.2) | |||
| Often | 67 (4.8) | 81 (7.2) | 1.5 (1.0 to 2.1) | 14 (6.6) | 0.8 (0.4 to 1.5) | |||
| Most times | 58 (4.1) | 25 (2.2) | 0.6 (0.4 to 1.1) | 12 (5.6) | 0.8 (0.4 to 1.7) | |||
| Characteristic . | No. of control subjects (%) . | Case patients . | . | . | . | |||
|---|---|---|---|---|---|---|---|---|
| . | . | Cancer of the oral cavity . | . | Cancer of the oropharynx . | . | |||
| . | . | No. (%) . | OR† (95% CI) . | No. (%) . | OR† (95% CI) . | |||
| Sex | ||||||||
| Male | 1078 (62.2) | 880 (62.2) | 214 (83.9) | |||||
| Female | 654 (37.8) | 535 (37.8) | 41 (16.1) | |||||
| Age, y | ||||||||
| ≤44 | 342 (19.7) | 177 (12.5) | 26 (10.2) | |||||
| 45–54 | 417 (24.1) | 319 (22.5) | 59 (23.1) | |||||
| 55–64 | 485 (28.0) | 422 (29.8) | 90 (35.3) | |||||
| ≥65 | 488 (28.2) | 497 (35.1) | 80 (31.4) | |||||
| No. of cigarettes per day‡ | ||||||||
| Never | 891 (51.8) | 542 (38.5) | 1.0 (referent) | 23 (9.3) | 1.0 (referent) | |||
| 1–5 | 106 (6.2) | 71 (5.0) | 1.4 (0.9 to 2.0) | 8 (3.2) | 2.4 (1.0 to 5.7) | |||
| 6–10 | 161 (9.4) | 121 (8.6) | 1.9 (1.4 to 2.6) | 25 (10.1) | 4.9 (2.6 to 9.2) | |||
| 11–15 | 96 (5.6) | 93 (6.6) | 2.9 (2.0 to 4.1) | 25 (10.1) | 7.0 (3.6 to 13.4) | |||
| 16–20 | 186 (10.8) | 208 (14.8) | 3.7 (2.8 to 5.0) | 46 (18.6) | 6.9 (3.8 to 12.5) | |||
| 21–30 | 157 (9.1) | 207 (14.7) | 4.5 (3.3 to 6.1) | 62 (25.1) | 13.2 (7.4 to 23.6) | |||
| >30 | 124 (7.2) | 167 (11.9) | 4.7 (3.4 to 6.6) | 58 (23.5) | 15.6 (8.5 to 28.8) | |||
| No. of alcoholic drinks per day§ | ||||||||
| Never drinker | 590 (43.0) | 388 (35.3) | 1.0 (referent) | 38 (15.9) | 1.0 (referent) | |||
| ≤4 | 605 (44.1) | 438 (39.8) | 1.3 (1.0 to 1.6) | 87 (36.4) | 1.2 (0.7 to 1.9) | |||
| 5–6 | 54 (3.9) | 79 (7.2) | 2.7 (1.7 to 4.2) | 24 (10.0) | 2.8 (1.4 to 5.6) | |||
| 7–10 | 58 (4.2) | 87 (7.9) | 2.9 (1.9 to 4.5) | 41 (17.2) | 4.8 (2.5 to 9.2) | |||
| 11–15 | 31 (2.3) | 51 (4.6) | 3.6 (2.1 to 6.1) | 25 (10.5) | 6.1 (2.9 to 12.9) | |||
| >15 | 33 (2.4) | 57 (5.2) | 3.3 (2.0 to 5.5) | 24 (10.0) | 6.0 (2.9 to 12.3) | |||
| No. of paan chewing units per day‖ | ||||||||
| Never chewer | 483 (84.0) | 139 (25.7) | 1.0 (referent) | 27 (81.8) | 1.0 (referent) | |||
| 1–5 | 65 (11.3) | 242 (44.8) | 14.5 (10.1 to 20.7) | 3 (9.1) | 0.6 (0.2 to 2.1) | |||
| 6–10 | 19 (3.3) | 116 (21.5) | 25.8 (15.1 to 44.4) | 2 (6.1) | 2.0 (0.4 to 10.0) | |||
| >10 | 8 (1.4) | 43 (8.0) | 21.7 (9.7 to 48.5) | 1 (3.0) | 4.5 (0.5 to 43.7) | |||
| Lifetime No. of sexual partners¶ | ||||||||
| 0–1 | 936 (60.9) | 807 (63.0) | 1.0 (referent) | 82 (35.7) | 1.0 (referent) | |||
| 2–5 | 256 (16.6) | 235 (18.3) | 0.9 (0.7 to 1.2) | 54 (23.5) | 1.1 (0.7 to 1.7) | |||
| 6–10 | 119 (7.7) | 88 (6.9) | 0.7 (0.5 to 1.0) | 28 (12.2) | 1.0 (0.6 to 1.8) | |||
| 11–20 | 88 (5.7) | 75 (5.9) | 0.8 (0.5 to 1.2) | 26 (11.3) | 1.1 (0.6 to 2.0) | |||
| 21–50 | 90 (5.9) | 44 (3.4) | 0.5 (0.3 to 0.7) | 23 (10.0) | 1.2 (0.7 to 2.2) | |||
| 51–100 | 27 (1.8) | 11 (0.9) | 0.4 (0.2 to 0.8) | 7 (3.0) | 1.0 (0.4 to 2.5) | |||
| >100 | 22 (1.4) | 21 (1.6) | 0.8 (0.4 to 1.6) | 10 (4.3) | 1.6 (0.7 to 3.9) | |||
| Frequency of oral sex# | ||||||||
| No oral sex | 1063 (75.7) | 881 (78.0) | 1.0 (referent) | 141 (66.2) | 1.0 (referent) | |||
| Occasionally | 216 (15.4) | 143 (12.7) | 0.9 (0.7 to 1.1) | 46 (21.6) | 0.8 (0.5 to 1.2) | |||
| Often | 67 (4.8) | 81 (7.2) | 1.5 (1.0 to 2.1) | 14 (6.6) | 0.8 (0.4 to 1.5) | |||
| Most times | 58 (4.1) | 25 (2.2) | 0.6 (0.4 to 1.1) | 12 (5.6) | 0.8 (0.4 to 1.7) | |||
OR = odds ratio; CI = confidence interval.
ORs adjusted for age, sex, center, smoking tobacco, chewing tobacco, and drinking alcohol, as appropriate.
Unknowns excluded (11 control subjects, 14 case patients).
Excludes subjects from Bangalore, India, and Sudan from whom information on amount of alcohol consumed was not obtained. Unknowns excluded (10 control subjects, 17 case patients).
Restricted to Indian subjects. Unknowns excluded (seven control subjects, nine case patients).
Excludes subjects from Northern Ireland from whom information on sexual behavior was not obtained and unknowns (144 control subjects and 89 case patients).
Excludes subjects from Northern Ireland from whom information on sexual behavior was not obtained and other unknowns (278 control subjects and 257 case patients).
Characteristics of case patients and control subjects and risks associated with tobacco smoking, paan chewing, alcohol drinking, and sexual behavior*
| Characteristic . | No. of control subjects (%) . | Case patients . | . | . | . | |||
|---|---|---|---|---|---|---|---|---|
| . | . | Cancer of the oral cavity . | . | Cancer of the oropharynx . | . | |||
| . | . | No. (%) . | OR† (95% CI) . | No. (%) . | OR† (95% CI) . | |||
| Sex | ||||||||
| Male | 1078 (62.2) | 880 (62.2) | 214 (83.9) | |||||
| Female | 654 (37.8) | 535 (37.8) | 41 (16.1) | |||||
| Age, y | ||||||||
| ≤44 | 342 (19.7) | 177 (12.5) | 26 (10.2) | |||||
| 45–54 | 417 (24.1) | 319 (22.5) | 59 (23.1) | |||||
| 55–64 | 485 (28.0) | 422 (29.8) | 90 (35.3) | |||||
| ≥65 | 488 (28.2) | 497 (35.1) | 80 (31.4) | |||||
| No. of cigarettes per day‡ | ||||||||
| Never | 891 (51.8) | 542 (38.5) | 1.0 (referent) | 23 (9.3) | 1.0 (referent) | |||
| 1–5 | 106 (6.2) | 71 (5.0) | 1.4 (0.9 to 2.0) | 8 (3.2) | 2.4 (1.0 to 5.7) | |||
| 6–10 | 161 (9.4) | 121 (8.6) | 1.9 (1.4 to 2.6) | 25 (10.1) | 4.9 (2.6 to 9.2) | |||
| 11–15 | 96 (5.6) | 93 (6.6) | 2.9 (2.0 to 4.1) | 25 (10.1) | 7.0 (3.6 to 13.4) | |||
| 16–20 | 186 (10.8) | 208 (14.8) | 3.7 (2.8 to 5.0) | 46 (18.6) | 6.9 (3.8 to 12.5) | |||
| 21–30 | 157 (9.1) | 207 (14.7) | 4.5 (3.3 to 6.1) | 62 (25.1) | 13.2 (7.4 to 23.6) | |||
| >30 | 124 (7.2) | 167 (11.9) | 4.7 (3.4 to 6.6) | 58 (23.5) | 15.6 (8.5 to 28.8) | |||
| No. of alcoholic drinks per day§ | ||||||||
| Never drinker | 590 (43.0) | 388 (35.3) | 1.0 (referent) | 38 (15.9) | 1.0 (referent) | |||
| ≤4 | 605 (44.1) | 438 (39.8) | 1.3 (1.0 to 1.6) | 87 (36.4) | 1.2 (0.7 to 1.9) | |||
| 5–6 | 54 (3.9) | 79 (7.2) | 2.7 (1.7 to 4.2) | 24 (10.0) | 2.8 (1.4 to 5.6) | |||
| 7–10 | 58 (4.2) | 87 (7.9) | 2.9 (1.9 to 4.5) | 41 (17.2) | 4.8 (2.5 to 9.2) | |||
| 11–15 | 31 (2.3) | 51 (4.6) | 3.6 (2.1 to 6.1) | 25 (10.5) | 6.1 (2.9 to 12.9) | |||
| >15 | 33 (2.4) | 57 (5.2) | 3.3 (2.0 to 5.5) | 24 (10.0) | 6.0 (2.9 to 12.3) | |||
| No. of paan chewing units per day‖ | ||||||||
| Never chewer | 483 (84.0) | 139 (25.7) | 1.0 (referent) | 27 (81.8) | 1.0 (referent) | |||
| 1–5 | 65 (11.3) | 242 (44.8) | 14.5 (10.1 to 20.7) | 3 (9.1) | 0.6 (0.2 to 2.1) | |||
| 6–10 | 19 (3.3) | 116 (21.5) | 25.8 (15.1 to 44.4) | 2 (6.1) | 2.0 (0.4 to 10.0) | |||
| >10 | 8 (1.4) | 43 (8.0) | 21.7 (9.7 to 48.5) | 1 (3.0) | 4.5 (0.5 to 43.7) | |||
| Lifetime No. of sexual partners¶ | ||||||||
| 0–1 | 936 (60.9) | 807 (63.0) | 1.0 (referent) | 82 (35.7) | 1.0 (referent) | |||
| 2–5 | 256 (16.6) | 235 (18.3) | 0.9 (0.7 to 1.2) | 54 (23.5) | 1.1 (0.7 to 1.7) | |||
| 6–10 | 119 (7.7) | 88 (6.9) | 0.7 (0.5 to 1.0) | 28 (12.2) | 1.0 (0.6 to 1.8) | |||
| 11–20 | 88 (5.7) | 75 (5.9) | 0.8 (0.5 to 1.2) | 26 (11.3) | 1.1 (0.6 to 2.0) | |||
| 21–50 | 90 (5.9) | 44 (3.4) | 0.5 (0.3 to 0.7) | 23 (10.0) | 1.2 (0.7 to 2.2) | |||
| 51–100 | 27 (1.8) | 11 (0.9) | 0.4 (0.2 to 0.8) | 7 (3.0) | 1.0 (0.4 to 2.5) | |||
| >100 | 22 (1.4) | 21 (1.6) | 0.8 (0.4 to 1.6) | 10 (4.3) | 1.6 (0.7 to 3.9) | |||
| Frequency of oral sex# | ||||||||
| No oral sex | 1063 (75.7) | 881 (78.0) | 1.0 (referent) | 141 (66.2) | 1.0 (referent) | |||
| Occasionally | 216 (15.4) | 143 (12.7) | 0.9 (0.7 to 1.1) | 46 (21.6) | 0.8 (0.5 to 1.2) | |||
| Often | 67 (4.8) | 81 (7.2) | 1.5 (1.0 to 2.1) | 14 (6.6) | 0.8 (0.4 to 1.5) | |||
| Most times | 58 (4.1) | 25 (2.2) | 0.6 (0.4 to 1.1) | 12 (5.6) | 0.8 (0.4 to 1.7) | |||
| Characteristic . | No. of control subjects (%) . | Case patients . | . | . | . | |||
|---|---|---|---|---|---|---|---|---|
| . | . | Cancer of the oral cavity . | . | Cancer of the oropharynx . | . | |||
| . | . | No. (%) . | OR† (95% CI) . | No. (%) . | OR† (95% CI) . | |||
| Sex | ||||||||
| Male | 1078 (62.2) | 880 (62.2) | 214 (83.9) | |||||
| Female | 654 (37.8) | 535 (37.8) | 41 (16.1) | |||||
| Age, y | ||||||||
| ≤44 | 342 (19.7) | 177 (12.5) | 26 (10.2) | |||||
| 45–54 | 417 (24.1) | 319 (22.5) | 59 (23.1) | |||||
| 55–64 | 485 (28.0) | 422 (29.8) | 90 (35.3) | |||||
| ≥65 | 488 (28.2) | 497 (35.1) | 80 (31.4) | |||||
| No. of cigarettes per day‡ | ||||||||
| Never | 891 (51.8) | 542 (38.5) | 1.0 (referent) | 23 (9.3) | 1.0 (referent) | |||
| 1–5 | 106 (6.2) | 71 (5.0) | 1.4 (0.9 to 2.0) | 8 (3.2) | 2.4 (1.0 to 5.7) | |||
| 6–10 | 161 (9.4) | 121 (8.6) | 1.9 (1.4 to 2.6) | 25 (10.1) | 4.9 (2.6 to 9.2) | |||
| 11–15 | 96 (5.6) | 93 (6.6) | 2.9 (2.0 to 4.1) | 25 (10.1) | 7.0 (3.6 to 13.4) | |||
| 16–20 | 186 (10.8) | 208 (14.8) | 3.7 (2.8 to 5.0) | 46 (18.6) | 6.9 (3.8 to 12.5) | |||
| 21–30 | 157 (9.1) | 207 (14.7) | 4.5 (3.3 to 6.1) | 62 (25.1) | 13.2 (7.4 to 23.6) | |||
| >30 | 124 (7.2) | 167 (11.9) | 4.7 (3.4 to 6.6) | 58 (23.5) | 15.6 (8.5 to 28.8) | |||
| No. of alcoholic drinks per day§ | ||||||||
| Never drinker | 590 (43.0) | 388 (35.3) | 1.0 (referent) | 38 (15.9) | 1.0 (referent) | |||
| ≤4 | 605 (44.1) | 438 (39.8) | 1.3 (1.0 to 1.6) | 87 (36.4) | 1.2 (0.7 to 1.9) | |||
| 5–6 | 54 (3.9) | 79 (7.2) | 2.7 (1.7 to 4.2) | 24 (10.0) | 2.8 (1.4 to 5.6) | |||
| 7–10 | 58 (4.2) | 87 (7.9) | 2.9 (1.9 to 4.5) | 41 (17.2) | 4.8 (2.5 to 9.2) | |||
| 11–15 | 31 (2.3) | 51 (4.6) | 3.6 (2.1 to 6.1) | 25 (10.5) | 6.1 (2.9 to 12.9) | |||
| >15 | 33 (2.4) | 57 (5.2) | 3.3 (2.0 to 5.5) | 24 (10.0) | 6.0 (2.9 to 12.3) | |||
| No. of paan chewing units per day‖ | ||||||||
| Never chewer | 483 (84.0) | 139 (25.7) | 1.0 (referent) | 27 (81.8) | 1.0 (referent) | |||
| 1–5 | 65 (11.3) | 242 (44.8) | 14.5 (10.1 to 20.7) | 3 (9.1) | 0.6 (0.2 to 2.1) | |||
| 6–10 | 19 (3.3) | 116 (21.5) | 25.8 (15.1 to 44.4) | 2 (6.1) | 2.0 (0.4 to 10.0) | |||
| >10 | 8 (1.4) | 43 (8.0) | 21.7 (9.7 to 48.5) | 1 (3.0) | 4.5 (0.5 to 43.7) | |||
| Lifetime No. of sexual partners¶ | ||||||||
| 0–1 | 936 (60.9) | 807 (63.0) | 1.0 (referent) | 82 (35.7) | 1.0 (referent) | |||
| 2–5 | 256 (16.6) | 235 (18.3) | 0.9 (0.7 to 1.2) | 54 (23.5) | 1.1 (0.7 to 1.7) | |||
| 6–10 | 119 (7.7) | 88 (6.9) | 0.7 (0.5 to 1.0) | 28 (12.2) | 1.0 (0.6 to 1.8) | |||
| 11–20 | 88 (5.7) | 75 (5.9) | 0.8 (0.5 to 1.2) | 26 (11.3) | 1.1 (0.6 to 2.0) | |||
| 21–50 | 90 (5.9) | 44 (3.4) | 0.5 (0.3 to 0.7) | 23 (10.0) | 1.2 (0.7 to 2.2) | |||
| 51–100 | 27 (1.8) | 11 (0.9) | 0.4 (0.2 to 0.8) | 7 (3.0) | 1.0 (0.4 to 2.5) | |||
| >100 | 22 (1.4) | 21 (1.6) | 0.8 (0.4 to 1.6) | 10 (4.3) | 1.6 (0.7 to 3.9) | |||
| Frequency of oral sex# | ||||||||
| No oral sex | 1063 (75.7) | 881 (78.0) | 1.0 (referent) | 141 (66.2) | 1.0 (referent) | |||
| Occasionally | 216 (15.4) | 143 (12.7) | 0.9 (0.7 to 1.1) | 46 (21.6) | 0.8 (0.5 to 1.2) | |||
| Often | 67 (4.8) | 81 (7.2) | 1.5 (1.0 to 2.1) | 14 (6.6) | 0.8 (0.4 to 1.5) | |||
| Most times | 58 (4.1) | 25 (2.2) | 0.6 (0.4 to 1.1) | 12 (5.6) | 0.8 (0.4 to 1.7) | |||
OR = odds ratio; CI = confidence interval.
ORs adjusted for age, sex, center, smoking tobacco, chewing tobacco, and drinking alcohol, as appropriate.
Unknowns excluded (11 control subjects, 14 case patients).
Excludes subjects from Bangalore, India, and Sudan from whom information on amount of alcohol consumed was not obtained. Unknowns excluded (10 control subjects, 17 case patients).
Restricted to Indian subjects. Unknowns excluded (seven control subjects, nine case patients).
Excludes subjects from Northern Ireland from whom information on sexual behavior was not obtained and unknowns (144 control subjects and 89 case patients).
Excludes subjects from Northern Ireland from whom information on sexual behavior was not obtained and other unknowns (278 control subjects and 257 case patients).
Risk associated with selected human papillomavirus (HPV) markers and topographic sites*
| HPV marker . | Control subjects, No. (%) . | Cancer of the oral cavity: case patients vs. control subjects . | . | Cancer of the oropharynx: case patients vs. control subjects . | . | Cancer of the oropharynx vs. cancer of the oral cavity in case patients . | ||
|---|---|---|---|---|---|---|---|---|
| . | . | No. (%) . | OR (95% CI) . | No. (%) . | OR (95% CI) . | OR (95% CI) . | ||
| HPV DNA in biopsy specimens | ||||||||
| Negative | 736 (96.1) | 116 (81.7) | ||||||
| Positive | 30 (3.9) | 26 (18.3) | 4.9 (2.6 to 9.1) | |||||
| HPV DNA in cells | ||||||||
| Negative | 571 (93.1) | 487 (95.3) | 1.0 (referent) | 82 (91.1) | 1.0 (referent) | 1.0 (referent) | ||
| Positive | 42 (6.9) | 24 (4.7) | 0.6 (0.3 to 1.1) | 8 (8.9) | 1.0 (0.4 to 2.5) | 2.0 (0.7 to 5.1) | ||
| HPV16 L1 antibodies | ||||||||
| Negative | 1436 (94.0) | 1184 (91.1) | 1.0 (referent) | 206 (86.6) | 1.0 (referent) | 1.0 (referent) | ||
| Positive | 91 (6.0) | 115 (8.9) | 1.5 (1.1 to 2.1) | 32 (13.4) | 3.5 (2.1 to 5.9) | 1.9 (1.2 to 3.0) | ||
| HPV16 E6 antibodies | ||||||||
| Negative | 1563 (98.9) | 1285 (97.4) | 1.0 (referent) | 219 (90.1) | 1.0 (referent) | 1.0 (referent) | ||
| Positive | 18 (1.1) | 34 (2.6) | 2.6 (1.4 to 5.0) | 24 (9.9) | 9.9 (4.7 to 20.7) | 4.4 (2.3 to 8.2) | ||
| HPV16 E7 antibodies | ||||||||
| Negative | 1571 (99.4) | 1286 (97.5) | 1.0 (referent) | 222 (91.4) | 1.0 (referent) | 1.0 (referent) | ||
| Positive | 10 (0.6) | 33 (2.5) | 3.4 (1.6 to 7.3) | 21 (8.6) | 19.0 (7.5 to 47.8) | 4.1 (2.1 to 8.1) | ||
| HPV16 E6 or E7 antibodies | ||||||||
| Negative | 1555 (98.4) | 1258 (95.4) | 1.0 (referent) | 214 (88.1) | 1.0 (referent) | 1.0 (referent) | ||
| One positive | 24 (1.5) | 55 (4.2) | 2.7 (1.6 to 4.7) | 13 (5.3) | 4.5 (2.0 to 10.1) | 1.9 (0.9 to 3.7) | ||
| Either or both positive | 26 (1.6) | 61 (4.6) | 2.9 (1.7 to 4.8) | 29 (11.9) | 9.2 (4.8 to 17.7) | 3.3 (1.9 to 5.6) | ||
| Both positive | 2 (0.1) | 6 (0.5) | 4.3 (0.8 to 23.2) | 16 (6.6) | 67.1 (12.9 to 348.2) | 13.5 (4.4 to 41.1) | ||
| HPV marker . | Control subjects, No. (%) . | Cancer of the oral cavity: case patients vs. control subjects . | . | Cancer of the oropharynx: case patients vs. control subjects . | . | Cancer of the oropharynx vs. cancer of the oral cavity in case patients . | ||
|---|---|---|---|---|---|---|---|---|
| . | . | No. (%) . | OR (95% CI) . | No. (%) . | OR (95% CI) . | OR (95% CI) . | ||
| HPV DNA in biopsy specimens | ||||||||
| Negative | 736 (96.1) | 116 (81.7) | ||||||
| Positive | 30 (3.9) | 26 (18.3) | 4.9 (2.6 to 9.1) | |||||
| HPV DNA in cells | ||||||||
| Negative | 571 (93.1) | 487 (95.3) | 1.0 (referent) | 82 (91.1) | 1.0 (referent) | 1.0 (referent) | ||
| Positive | 42 (6.9) | 24 (4.7) | 0.6 (0.3 to 1.1) | 8 (8.9) | 1.0 (0.4 to 2.5) | 2.0 (0.7 to 5.1) | ||
| HPV16 L1 antibodies | ||||||||
| Negative | 1436 (94.0) | 1184 (91.1) | 1.0 (referent) | 206 (86.6) | 1.0 (referent) | 1.0 (referent) | ||
| Positive | 91 (6.0) | 115 (8.9) | 1.5 (1.1 to 2.1) | 32 (13.4) | 3.5 (2.1 to 5.9) | 1.9 (1.2 to 3.0) | ||
| HPV16 E6 antibodies | ||||||||
| Negative | 1563 (98.9) | 1285 (97.4) | 1.0 (referent) | 219 (90.1) | 1.0 (referent) | 1.0 (referent) | ||
| Positive | 18 (1.1) | 34 (2.6) | 2.6 (1.4 to 5.0) | 24 (9.9) | 9.9 (4.7 to 20.7) | 4.4 (2.3 to 8.2) | ||
| HPV16 E7 antibodies | ||||||||
| Negative | 1571 (99.4) | 1286 (97.5) | 1.0 (referent) | 222 (91.4) | 1.0 (referent) | 1.0 (referent) | ||
| Positive | 10 (0.6) | 33 (2.5) | 3.4 (1.6 to 7.3) | 21 (8.6) | 19.0 (7.5 to 47.8) | 4.1 (2.1 to 8.1) | ||
| HPV16 E6 or E7 antibodies | ||||||||
| Negative | 1555 (98.4) | 1258 (95.4) | 1.0 (referent) | 214 (88.1) | 1.0 (referent) | 1.0 (referent) | ||
| One positive | 24 (1.5) | 55 (4.2) | 2.7 (1.6 to 4.7) | 13 (5.3) | 4.5 (2.0 to 10.1) | 1.9 (0.9 to 3.7) | ||
| Either or both positive | 26 (1.6) | 61 (4.6) | 2.9 (1.7 to 4.8) | 29 (11.9) | 9.2 (4.8 to 17.7) | 3.3 (1.9 to 5.6) | ||
| Both positive | 2 (0.1) | 6 (0.5) | 4.3 (0.8 to 23.2) | 16 (6.6) | 67.1 (12.9 to 348.2) | 13.5 (4.4 to 41.1) | ||
Models adjusted for country, sex, age group, smoking tobacco, drinking alcohol, and paan chewing. Subjects with unknown values were excluded. Values differ from those expected because categories are not mutually exclusive. OR = odds ratio; CI = confidence interval.
Risk associated with selected human papillomavirus (HPV) markers and topographic sites*
| HPV marker . | Control subjects, No. (%) . | Cancer of the oral cavity: case patients vs. control subjects . | . | Cancer of the oropharynx: case patients vs. control subjects . | . | Cancer of the oropharynx vs. cancer of the oral cavity in case patients . | ||
|---|---|---|---|---|---|---|---|---|
| . | . | No. (%) . | OR (95% CI) . | No. (%) . | OR (95% CI) . | OR (95% CI) . | ||
| HPV DNA in biopsy specimens | ||||||||
| Negative | 736 (96.1) | 116 (81.7) | ||||||
| Positive | 30 (3.9) | 26 (18.3) | 4.9 (2.6 to 9.1) | |||||
| HPV DNA in cells | ||||||||
| Negative | 571 (93.1) | 487 (95.3) | 1.0 (referent) | 82 (91.1) | 1.0 (referent) | 1.0 (referent) | ||
| Positive | 42 (6.9) | 24 (4.7) | 0.6 (0.3 to 1.1) | 8 (8.9) | 1.0 (0.4 to 2.5) | 2.0 (0.7 to 5.1) | ||
| HPV16 L1 antibodies | ||||||||
| Negative | 1436 (94.0) | 1184 (91.1) | 1.0 (referent) | 206 (86.6) | 1.0 (referent) | 1.0 (referent) | ||
| Positive | 91 (6.0) | 115 (8.9) | 1.5 (1.1 to 2.1) | 32 (13.4) | 3.5 (2.1 to 5.9) | 1.9 (1.2 to 3.0) | ||
| HPV16 E6 antibodies | ||||||||
| Negative | 1563 (98.9) | 1285 (97.4) | 1.0 (referent) | 219 (90.1) | 1.0 (referent) | 1.0 (referent) | ||
| Positive | 18 (1.1) | 34 (2.6) | 2.6 (1.4 to 5.0) | 24 (9.9) | 9.9 (4.7 to 20.7) | 4.4 (2.3 to 8.2) | ||
| HPV16 E7 antibodies | ||||||||
| Negative | 1571 (99.4) | 1286 (97.5) | 1.0 (referent) | 222 (91.4) | 1.0 (referent) | 1.0 (referent) | ||
| Positive | 10 (0.6) | 33 (2.5) | 3.4 (1.6 to 7.3) | 21 (8.6) | 19.0 (7.5 to 47.8) | 4.1 (2.1 to 8.1) | ||
| HPV16 E6 or E7 antibodies | ||||||||
| Negative | 1555 (98.4) | 1258 (95.4) | 1.0 (referent) | 214 (88.1) | 1.0 (referent) | 1.0 (referent) | ||
| One positive | 24 (1.5) | 55 (4.2) | 2.7 (1.6 to 4.7) | 13 (5.3) | 4.5 (2.0 to 10.1) | 1.9 (0.9 to 3.7) | ||
| Either or both positive | 26 (1.6) | 61 (4.6) | 2.9 (1.7 to 4.8) | 29 (11.9) | 9.2 (4.8 to 17.7) | 3.3 (1.9 to 5.6) | ||
| Both positive | 2 (0.1) | 6 (0.5) | 4.3 (0.8 to 23.2) | 16 (6.6) | 67.1 (12.9 to 348.2) | 13.5 (4.4 to 41.1) | ||
| HPV marker . | Control subjects, No. (%) . | Cancer of the oral cavity: case patients vs. control subjects . | . | Cancer of the oropharynx: case patients vs. control subjects . | . | Cancer of the oropharynx vs. cancer of the oral cavity in case patients . | ||
|---|---|---|---|---|---|---|---|---|
| . | . | No. (%) . | OR (95% CI) . | No. (%) . | OR (95% CI) . | OR (95% CI) . | ||
| HPV DNA in biopsy specimens | ||||||||
| Negative | 736 (96.1) | 116 (81.7) | ||||||
| Positive | 30 (3.9) | 26 (18.3) | 4.9 (2.6 to 9.1) | |||||
| HPV DNA in cells | ||||||||
| Negative | 571 (93.1) | 487 (95.3) | 1.0 (referent) | 82 (91.1) | 1.0 (referent) | 1.0 (referent) | ||
| Positive | 42 (6.9) | 24 (4.7) | 0.6 (0.3 to 1.1) | 8 (8.9) | 1.0 (0.4 to 2.5) | 2.0 (0.7 to 5.1) | ||
| HPV16 L1 antibodies | ||||||||
| Negative | 1436 (94.0) | 1184 (91.1) | 1.0 (referent) | 206 (86.6) | 1.0 (referent) | 1.0 (referent) | ||
| Positive | 91 (6.0) | 115 (8.9) | 1.5 (1.1 to 2.1) | 32 (13.4) | 3.5 (2.1 to 5.9) | 1.9 (1.2 to 3.0) | ||
| HPV16 E6 antibodies | ||||||||
| Negative | 1563 (98.9) | 1285 (97.4) | 1.0 (referent) | 219 (90.1) | 1.0 (referent) | 1.0 (referent) | ||
| Positive | 18 (1.1) | 34 (2.6) | 2.6 (1.4 to 5.0) | 24 (9.9) | 9.9 (4.7 to 20.7) | 4.4 (2.3 to 8.2) | ||
| HPV16 E7 antibodies | ||||||||
| Negative | 1571 (99.4) | 1286 (97.5) | 1.0 (referent) | 222 (91.4) | 1.0 (referent) | 1.0 (referent) | ||
| Positive | 10 (0.6) | 33 (2.5) | 3.4 (1.6 to 7.3) | 21 (8.6) | 19.0 (7.5 to 47.8) | 4.1 (2.1 to 8.1) | ||
| HPV16 E6 or E7 antibodies | ||||||||
| Negative | 1555 (98.4) | 1258 (95.4) | 1.0 (referent) | 214 (88.1) | 1.0 (referent) | 1.0 (referent) | ||
| One positive | 24 (1.5) | 55 (4.2) | 2.7 (1.6 to 4.7) | 13 (5.3) | 4.5 (2.0 to 10.1) | 1.9 (0.9 to 3.7) | ||
| Either or both positive | 26 (1.6) | 61 (4.6) | 2.9 (1.7 to 4.8) | 29 (11.9) | 9.2 (4.8 to 17.7) | 3.3 (1.9 to 5.6) | ||
| Both positive | 2 (0.1) | 6 (0.5) | 4.3 (0.8 to 23.2) | 16 (6.6) | 67.1 (12.9 to 348.2) | 13.5 (4.4 to 41.1) | ||
Models adjusted for country, sex, age group, smoking tobacco, drinking alcohol, and paan chewing. Subjects with unknown values were excluded. Values differ from those expected because categories are not mutually exclusive. OR = odds ratio; CI = confidence interval.
Prevalence of immunoglobulin G (IgG) antibodies against HPV16 E6 or E7 and HPV16 L1 by HPV DNA status among case patients*
| Antibody . | HPV DNA—negative . | . | HPV DNA—positive . | . | HPV DNA unknown . | . | |||
|---|---|---|---|---|---|---|---|---|---|
| . | Oral cavity, No. (%) . | Oropharynx, No. (%) . | Oral cavity, No. (%) . | Oropharynx, No. (%) . | Oral cavity, No. (%) . | Oropharynx, No. (%) . | |||
| HPV16 L1 | |||||||||
| Negative | 617 (89.9) | 100 (92.6) | 22 (73.3) | 12 (48.0) | 545 (93.5) | 94 (89.5) | |||
| Positive | 69 (10.1) | 8 (7.4) | 8 (26.7) | 13 (52.0) | 38 (6.5) | 11 (10.5) | |||
| P* | .39 | .05 | .15 | ||||||
| HPV16 E6 or E7 | |||||||||
| Negative | 672 (96.1) | 107 (96.4) | 26 (86.7) | 9 (34.6) | 560 (94.9) | 98 (92.5) | |||
| Either or both positive | 27 (3.9) | 4 (3.6) | 4 (13.3) | 17 (65.4) | 30 (5.1) | 8 (7.5) | |||
| P* | .89 | <.001 | .30 | ||||||
| Antibody . | HPV DNA—negative . | . | HPV DNA—positive . | . | HPV DNA unknown . | . | |||
|---|---|---|---|---|---|---|---|---|---|
| . | Oral cavity, No. (%) . | Oropharynx, No. (%) . | Oral cavity, No. (%) . | Oropharynx, No. (%) . | Oral cavity, No. (%) . | Oropharynx, No. (%) . | |||
| HPV16 L1 | |||||||||
| Negative | 617 (89.9) | 100 (92.6) | 22 (73.3) | 12 (48.0) | 545 (93.5) | 94 (89.5) | |||
| Positive | 69 (10.1) | 8 (7.4) | 8 (26.7) | 13 (52.0) | 38 (6.5) | 11 (10.5) | |||
| P* | .39 | .05 | .15 | ||||||
| HPV16 E6 or E7 | |||||||||
| Negative | 672 (96.1) | 107 (96.4) | 26 (86.7) | 9 (34.6) | 560 (94.9) | 98 (92.5) | |||
| Either or both positive | 27 (3.9) | 4 (3.6) | 4 (13.3) | 17 (65.4) | 30 (5.1) | 8 (7.5) | |||
| P* | .89 | <.001 | .30 | ||||||
Two-sided χ2 test.
Prevalence of immunoglobulin G (IgG) antibodies against HPV16 E6 or E7 and HPV16 L1 by HPV DNA status among case patients*
| Antibody . | HPV DNA—negative . | . | HPV DNA—positive . | . | HPV DNA unknown . | . | |||
|---|---|---|---|---|---|---|---|---|---|
| . | Oral cavity, No. (%) . | Oropharynx, No. (%) . | Oral cavity, No. (%) . | Oropharynx, No. (%) . | Oral cavity, No. (%) . | Oropharynx, No. (%) . | |||
| HPV16 L1 | |||||||||
| Negative | 617 (89.9) | 100 (92.6) | 22 (73.3) | 12 (48.0) | 545 (93.5) | 94 (89.5) | |||
| Positive | 69 (10.1) | 8 (7.4) | 8 (26.7) | 13 (52.0) | 38 (6.5) | 11 (10.5) | |||
| P* | .39 | .05 | .15 | ||||||
| HPV16 E6 or E7 | |||||||||
| Negative | 672 (96.1) | 107 (96.4) | 26 (86.7) | 9 (34.6) | 560 (94.9) | 98 (92.5) | |||
| Either or both positive | 27 (3.9) | 4 (3.6) | 4 (13.3) | 17 (65.4) | 30 (5.1) | 8 (7.5) | |||
| P* | .89 | <.001 | .30 | ||||||
| Antibody . | HPV DNA—negative . | . | HPV DNA—positive . | . | HPV DNA unknown . | . | |||
|---|---|---|---|---|---|---|---|---|---|
| . | Oral cavity, No. (%) . | Oropharynx, No. (%) . | Oral cavity, No. (%) . | Oropharynx, No. (%) . | Oral cavity, No. (%) . | Oropharynx, No. (%) . | |||
| HPV16 L1 | |||||||||
| Negative | 617 (89.9) | 100 (92.6) | 22 (73.3) | 12 (48.0) | 545 (93.5) | 94 (89.5) | |||
| Positive | 69 (10.1) | 8 (7.4) | 8 (26.7) | 13 (52.0) | 38 (6.5) | 11 (10.5) | |||
| P* | .39 | .05 | .15 | ||||||
| HPV16 E6 or E7 | |||||||||
| Negative | 672 (96.1) | 107 (96.4) | 26 (86.7) | 9 (34.6) | 560 (94.9) | 98 (92.5) | |||
| Either or both positive | 27 (3.9) | 4 (3.6) | 4 (13.3) | 17 (65.4) | 30 (5.1) | 8 (7.5) | |||
| P* | .89 | <.001 | .30 | ||||||
Two-sided χ2 test.
Agreement between human papillomavirus (HPV) DNA detection in biopsies and cells among cancer case patients*
| HPV DNA in biopsy . | HPV DNA in cells . | . | . | ||
|---|---|---|---|---|---|
| . | No. negative . | No. positive . | Total No. . | ||
| No. negative | 314 | 15 | 329 | ||
| No. positive | 18 | 2 | 20 | ||
| Total No. | 332 | 17 | 349 | ||
| HPV DNA in biopsy . | HPV DNA in cells . | . | . | ||
|---|---|---|---|---|---|
| . | No. negative . | No. positive . | Total No. . | ||
| No. negative | 314 | 15 | 329 | ||
| No. positive | 18 | 2 | 20 | ||
| Total No. | 332 | 17 | 349 | ||
κ = 0.059 (95% confidence interval [CI] = −0.035 to 0.281). Sensitivity = 10% (95% CI = 1.9% to 29.5%). Specificity = 95.4% (95% CI = 94.9% to 96.6%).
Agreement between human papillomavirus (HPV) DNA detection in biopsies and cells among cancer case patients*
| HPV DNA in biopsy . | HPV DNA in cells . | . | . | ||
|---|---|---|---|---|---|
| . | No. negative . | No. positive . | Total No. . | ||
| No. negative | 314 | 15 | 329 | ||
| No. positive | 18 | 2 | 20 | ||
| Total No. | 332 | 17 | 349 | ||
| HPV DNA in biopsy . | HPV DNA in cells . | . | . | ||
|---|---|---|---|---|---|
| . | No. negative . | No. positive . | Total No. . | ||
| No. negative | 314 | 15 | 329 | ||
| No. positive | 18 | 2 | 20 | ||
| Total No. | 332 | 17 | 349 | ||
κ = 0.059 (95% confidence interval [CI] = −0.035 to 0.281). Sensitivity = 10% (95% CI = 1.9% to 29.5%). Specificity = 95.4% (95% CI = 94.9% to 96.6%).
Risk associated with smoking or chewing tobacco combined with detection of antibodies against human papillomavirus 16 (HPV16) L1 virus-like particles (VLPs) or combined with detection of HPV16 E6 or E7 antibodies*
| . | Tobacco smoking or paan chewing . | . | . | . | ||||
|---|---|---|---|---|---|---|---|---|
| . | Never . | . | Ever . | . | ||||
| . | OR (95% CI) . | No. of case patients/No. of control subjects . | OR (95% CI) . | No. of case patients/No. of control subjects . | ||||
| HPV16 L1 VLP antibodies | ||||||||
| Cancer of the oral cavity: case patients vs. control subjects | ||||||||
| Negative | 1.0 (referent) | 176/672 | 6.6 (5.3 to 8.2) | 1002/761 | ||||
| Positive | 1.3 (0.7 to 2.3) | 18/53 | 11.4 (7.4 to 17.6) | 95/38 | ||||
| P for departure from multiplicative model = .461 | ||||||||
| Cancer of the oropharynx: case patients vs. control subjects | ||||||||
| Negative | 1.0 (referent) | 12/672 | 9.2 (4.9 to 17.1) | 194/761 | ||||
| Positive | 6.7 (2.3 to 19.1) | 6/53 | 26.6 (11.9 to 59.4) | 26/38 | ||||
| P for departure from multiplicative model = .181 | ||||||||
| HPV16 E6 or E7 positivity | ||||||||
| Cancer of the oral cavity: case patients vs. control subjects | ||||||||
| Both negative | 1.0 (referent) | 187/740 | 6.7 (5.4 to 8.4) | 1063/812 | ||||
| Either or both positive | 6.7 (2.6 to 17.3) | 12/8 | 13.0 (7.2 to 23.5) | 49/18 | ||||
| P for departure from multiplicative model = .030 | ||||||||
| Cancer of the oropharynx: case patients vs. control subjects | ||||||||
| Both negative | 1.0 (referent) | 11/740 | 11.2 (5.9 to 21.4) | 203/812 | ||||
| Either or both positive | 64.5 (18.3 to 226.7) | 7/8 | 56.2 (22.5 to 140.4) | 22/18 | ||||
| P for departure from multiplicative model = .001 | ||||||||
| . | Tobacco smoking or paan chewing . | . | . | . | ||||
|---|---|---|---|---|---|---|---|---|
| . | Never . | . | Ever . | . | ||||
| . | OR (95% CI) . | No. of case patients/No. of control subjects . | OR (95% CI) . | No. of case patients/No. of control subjects . | ||||
| HPV16 L1 VLP antibodies | ||||||||
| Cancer of the oral cavity: case patients vs. control subjects | ||||||||
| Negative | 1.0 (referent) | 176/672 | 6.6 (5.3 to 8.2) | 1002/761 | ||||
| Positive | 1.3 (0.7 to 2.3) | 18/53 | 11.4 (7.4 to 17.6) | 95/38 | ||||
| P for departure from multiplicative model = .461 | ||||||||
| Cancer of the oropharynx: case patients vs. control subjects | ||||||||
| Negative | 1.0 (referent) | 12/672 | 9.2 (4.9 to 17.1) | 194/761 | ||||
| Positive | 6.7 (2.3 to 19.1) | 6/53 | 26.6 (11.9 to 59.4) | 26/38 | ||||
| P for departure from multiplicative model = .181 | ||||||||
| HPV16 E6 or E7 positivity | ||||||||
| Cancer of the oral cavity: case patients vs. control subjects | ||||||||
| Both negative | 1.0 (referent) | 187/740 | 6.7 (5.4 to 8.4) | 1063/812 | ||||
| Either or both positive | 6.7 (2.6 to 17.3) | 12/8 | 13.0 (7.2 to 23.5) | 49/18 | ||||
| P for departure from multiplicative model = .030 | ||||||||
| Cancer of the oropharynx: case patients vs. control subjects | ||||||||
| Both negative | 1.0 (referent) | 11/740 | 11.2 (5.9 to 21.4) | 203/812 | ||||
| Either or both positive | 64.5 (18.3 to 226.7) | 7/8 | 56.2 (22.5 to 140.4) | 22/18 | ||||
| P for departure from multiplicative model = .001 | ||||||||
Models adjusted for country, age, sex, and alcohol consumption status. OR = odds ratio; CI = confidence interval.
Risk associated with smoking or chewing tobacco combined with detection of antibodies against human papillomavirus 16 (HPV16) L1 virus-like particles (VLPs) or combined with detection of HPV16 E6 or E7 antibodies*
| . | Tobacco smoking or paan chewing . | . | . | . | ||||
|---|---|---|---|---|---|---|---|---|
| . | Never . | . | Ever . | . | ||||
| . | OR (95% CI) . | No. of case patients/No. of control subjects . | OR (95% CI) . | No. of case patients/No. of control subjects . | ||||
| HPV16 L1 VLP antibodies | ||||||||
| Cancer of the oral cavity: case patients vs. control subjects | ||||||||
| Negative | 1.0 (referent) | 176/672 | 6.6 (5.3 to 8.2) | 1002/761 | ||||
| Positive | 1.3 (0.7 to 2.3) | 18/53 | 11.4 (7.4 to 17.6) | 95/38 | ||||
| P for departure from multiplicative model = .461 | ||||||||
| Cancer of the oropharynx: case patients vs. control subjects | ||||||||
| Negative | 1.0 (referent) | 12/672 | 9.2 (4.9 to 17.1) | 194/761 | ||||
| Positive | 6.7 (2.3 to 19.1) | 6/53 | 26.6 (11.9 to 59.4) | 26/38 | ||||
| P for departure from multiplicative model = .181 | ||||||||
| HPV16 E6 or E7 positivity | ||||||||
| Cancer of the oral cavity: case patients vs. control subjects | ||||||||
| Both negative | 1.0 (referent) | 187/740 | 6.7 (5.4 to 8.4) | 1063/812 | ||||
| Either or both positive | 6.7 (2.6 to 17.3) | 12/8 | 13.0 (7.2 to 23.5) | 49/18 | ||||
| P for departure from multiplicative model = .030 | ||||||||
| Cancer of the oropharynx: case patients vs. control subjects | ||||||||
| Both negative | 1.0 (referent) | 11/740 | 11.2 (5.9 to 21.4) | 203/812 | ||||
| Either or both positive | 64.5 (18.3 to 226.7) | 7/8 | 56.2 (22.5 to 140.4) | 22/18 | ||||
| P for departure from multiplicative model = .001 | ||||||||
| . | Tobacco smoking or paan chewing . | . | . | . | ||||
|---|---|---|---|---|---|---|---|---|
| . | Never . | . | Ever . | . | ||||
| . | OR (95% CI) . | No. of case patients/No. of control subjects . | OR (95% CI) . | No. of case patients/No. of control subjects . | ||||
| HPV16 L1 VLP antibodies | ||||||||
| Cancer of the oral cavity: case patients vs. control subjects | ||||||||
| Negative | 1.0 (referent) | 176/672 | 6.6 (5.3 to 8.2) | 1002/761 | ||||
| Positive | 1.3 (0.7 to 2.3) | 18/53 | 11.4 (7.4 to 17.6) | 95/38 | ||||
| P for departure from multiplicative model = .461 | ||||||||
| Cancer of the oropharynx: case patients vs. control subjects | ||||||||
| Negative | 1.0 (referent) | 12/672 | 9.2 (4.9 to 17.1) | 194/761 | ||||
| Positive | 6.7 (2.3 to 19.1) | 6/53 | 26.6 (11.9 to 59.4) | 26/38 | ||||
| P for departure from multiplicative model = .181 | ||||||||
| HPV16 E6 or E7 positivity | ||||||||
| Cancer of the oral cavity: case patients vs. control subjects | ||||||||
| Both negative | 1.0 (referent) | 187/740 | 6.7 (5.4 to 8.4) | 1063/812 | ||||
| Either or both positive | 6.7 (2.6 to 17.3) | 12/8 | 13.0 (7.2 to 23.5) | 49/18 | ||||
| P for departure from multiplicative model = .030 | ||||||||
| Cancer of the oropharynx: case patients vs. control subjects | ||||||||
| Both negative | 1.0 (referent) | 11/740 | 11.2 (5.9 to 21.4) | 203/812 | ||||
| Either or both positive | 64.5 (18.3 to 226.7) | 7/8 | 56.2 (22.5 to 140.4) | 22/18 | ||||
| P for departure from multiplicative model = .001 | ||||||||
Models adjusted for country, age, sex, and alcohol consumption status. OR = odds ratio; CI = confidence interval.
Supported by grant S06 96202489 05F02 from Europe Against Cancer (to the International Agency for Research on Cancer, Lyon, France [N. Muñoz and R. Herrero]) and grants FIS 97/0662, FIS 01/1236, and BAE 01/5013 (to the Institut Català d’Oncologia, Barcelona, Spain [X. Castellsagué and F. Xavier Bosch]) from “Fondo de Investigaciones Sanitarias” (FIS), Madrid, Spain. Funding was also provided by the International Union Against Cancer (UICC) Yamagiwa-Yoshida Memorial International Cancer Study (to X. Castellsagué), the National Cancer Institute of Canada (to McGill University, Montreal, Quebec, Canada [E. Franco]), the Italian Association for Research on Cancer (to the Centro di Riferimento Oncologico di Aviano, Aviano, Italy [S. Franceschi]), and the Pan American Health Organization (to the Instituto Nacional de Oncologia y Radiobiologia, Havana, Cuba [L. Fernández]).
See “Appendix” for a list of additional members of the study group.
References
Bray F, Ferlay J, Parkin DM, Pisani P.
Franceschi S, Bidoli E, Herrero R, Muñoz N. Comparison of cancers of the oral cavity and pharynx worldwide: etiological clues.
Castellsagué X, Quintana MJ, Martínez MC, Nieto A, Sánchez MJ, Amparo J, et al. The role of type of tobacco and type of alcoholic beverage in oral carcinogenensis.
Garrote LF, Herrero R, Ortiz Reyes RM, Vaccarella S, Anta JL, Ferbeye L, et al. Risk factors for cancer of the oral cavity and oro-pharynx in Cuba.
Sanchez MJ, Martinez C, Nieto A, Castellsagué X, Quintana MJ, Bosch FX, et al. Oral and oropharyngeal cancer in Spain: influence of dietary patterns.
Talamini R, Vacarella S, Barbone F, Tavani A, La Vecchia C, Herrero R, et al. Oral hygiene, dentition, sexual habits and risk of oral cancer.
Bosch FX, Lorincz A, Muñoz N, Meijer CJ, Shah KV. The causal relation between HPV and cervical cancer.
Shah KV. Do human papillomavirus infections cause oral cancer?
Gillison ML, Koch WM, Capone RB, Spafford M, Westra WH, Wu L, et al. Evidence for a causal association between human papillomavirus and a subset of head and neck cancers.
Smith EM, Hoffman HT, Summersgill KS, Kirchner HL, Turek LP, Haugen TH. Human papillomavirus and risk of oral cancer.
Schwartz SM, Daling JR, Doody DR, Wipf GC, Carter JJ, Madeleine MM, et al. Oral cancer risk in relation to sexual history and evidence of HPV infection.
Franceschi S, Muñoz N, Snijders PJ, Walboomers WW. Human papillomavirus and cancers of the upper aerodigestive tract: a review of epidemiological and experimental evidence.
Mork J, Lie AK, Glattre E, Hallmans G, Jellum E, Koskela P, et al. Human papillomavirus infection as a risk factor for squamous-cell carcinoma of the head and neck.
Herrero R. Chapter 7: Human papillomavirus and cancer of the upper aerodigestive tract.
Lissowska J, Pilarska A, Pilarski P, Samolczyk-Wanyura D, Piekarczyk J, Bardin-Mikollajczak A, et al. Smoking, alcohol, diet, dentition and sexual practices in the epidemiology of oral cancer in Poland.
Balaram P, Shridar H, Rajkumar T, Vaccarella S, Herrero R, Nandakumar A, et al. Oral cancer in Southern India: the influence of smoking, drinking, paan chewing and oral hygiene.
Fleming ID, Cooper JS, Henson DE, Hutter RV, Kennedy BJ Murphy GP, et al., editors.
Jacobs MV, Snijders PJ, van den Brule AJ, Helmerhorst TJ, Meijer CJ, Walboomers JM. A general primer GP5+/GP6(+)-mediated PCR-enzyme immunoassay method for rapid detection of 14 high-risk and 6 low-risk human papillomavirus genotypes in cervical scrapings.
van Houten VM, Snijders PJ, van den Brekel MW, Kummer JA, Meijer CJ, van Leeuwen B, et al. Biological evidence that human papillomaviruses are etiologically involved in a subgroup of head and neck squamous cell carcinomas.
de Roda Husman AM, Snijders PJ, Stel HV, van den Brule AJ, Meijer CJ, Walboomers JM. Processing of long-stored archival cervical smears for human papillomavirus detection by the polymerase chain reaction.
van den Brule AJ, Meijer CJ, Bakels V, Kenemans P, Walboomers JM. Rapid detection of human papillomavirus in cervical scrapes by combined general primer-mediated and type-specific polymerase chain reaction.
Viscidi RP, Ahdieh-Grant L, Clayman B, Fox K, Massad LS, Cu-Uvin S, et al. Serum immunoglobulin G response to human papillomavirus type 16 virus-like particles in human immunodeficiency virus (HIV)-positive and risk-matched HIV-negative women.
Sehr P, Zumbach K, Pawlita M. A generic capture ELISA for recombinant proteins fused to glutathione S-transferase: validation for HPV serology.
Paz IB, Cook N, Odom-Maryon T, Xie Y, Wilczynski SP. Human papillomavirus (HPV) in head and neck cancer. An assocaition of HPV 16 with squamous cell carcinoma of Waldeyer’s tonsillar ring.
Miller CS, Johnstone BM. Human papillomavirus as a risk factor for oral squamous cell carcinoma: a meta-analysis.
Meschede W, Zumbach K, Braspenning J, Scheffner M, Benitez-Bribiesca L, Luande J, et al. Antibodies against early proteins of human papillomaviruses as diagnostic markers for invasive cervical cancer.
Stanley M. Antibody reactivity to HPV E6 and E7 oncoproteins and early diagnosis of invasive cervical cancer.
Lehtinen M, Pawlita M, Zumbach K, Lie K, Hakama M, Jellum E, et al. Evaluation of antibody response to HPV early proteins in women in whom cervical cancer developed one to 20 years later.
Rosales R, Lopez-Contreras M, Cortes RR. Antibodies against HPV type 16 and 18 E2, E6 and E7 proteins in sera: correlation with presence of papillomavirus DNA.
Zumbach K, Hoffman M, Kahn T, Bosch F, Gottschlich S, Gorogh T, et al. Antibodies against oncoproteins E6 and E7 of HPV types 16 and 18 in patients with head and neck squamous cell carcinoma.
Tomassino M, Accardi R, Caldeira S, Dong W, Malanchi I, Smet A, Zehbe I. The role of p53 in cervical carcinogenesis.
Wiest T, Schwarz E, Enders C, Flechtenmacher C, Boxch FX. Involvement of intact HPV16 E6/E7 gene expression in head and neck cancers with unaltered p53 status and perturbed pRB cell cycle control.
Wilczynski SP, Lin BT, Xie Y, Paz IB. Detection of human papillomavirus DNA and oncoprotein overexpression are associated with distinct morphological patterns of tonsillar squamous cell carcinoma.
Snijders PJ, Cromme FV, van den Brule AJ, Schrijnemakers HF, Snow GB, Meijer CJ, et al. Prevalence and expression of human papillomaviruses in tonsillar carcinomas, indicating a possible viral etiology.
Snijders PJ, Meijer CJ, van den Brule AJ, Schrijnemakers HF, Snow GB, Walboomers JM. Human papillomavirus (HPV) type 16 and 33 E6/E7 region transcripts in tonsillar carcinomas can originate from integrated and episomal HPV DNA.
Klussmann JP, Weissenborn SJ, Wieland U, Dries V, Kolligs J, Jungehuelsing M, et al. Prevalence, distribution, and viral load of human papillomavirus 16 DNA in tonsillar carcinomas.
Steenbergen RD, Hermsen MA, Walboomers JM, Joenje H, Arwert F, Meijer CJ, et al. Integrated human papillomavirus type 16 and loss of heterozygosity at 11q22 and 18q21 in an oral carcinoma and its derivative cell line.